Reply To:
Name - Reply Comment

By Kalani Kumarasinghe
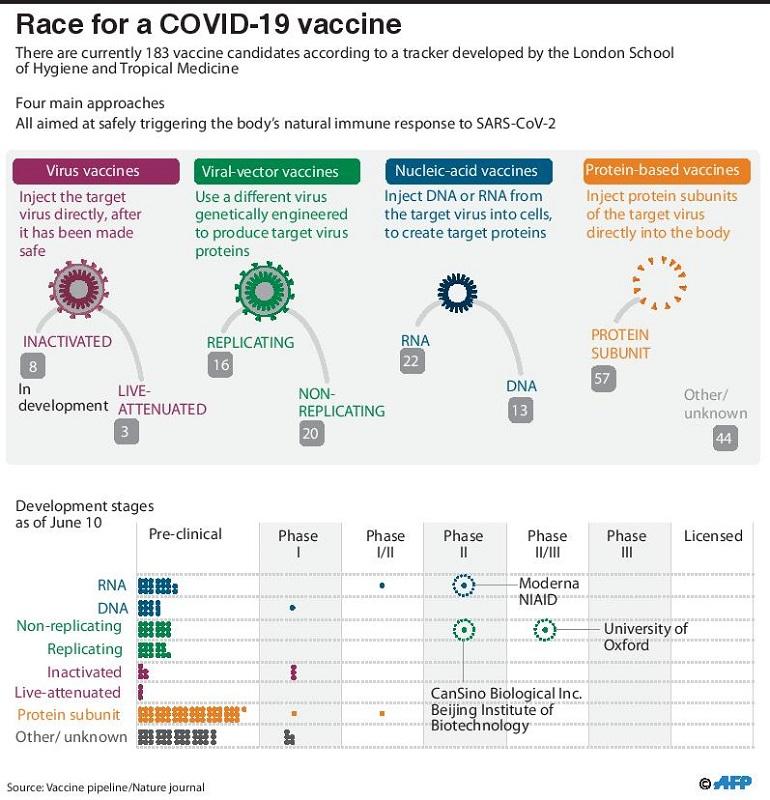
Governments, pharmaceutical companies and private investors are now racing to develop a vaccine in record time against a raging global pandemic. According to the Vaccine Centre of the London School of Hygiene and Tropical Medicine, there are currently 183 candidate vaccines in the pipeline against COVID-19. While some of these researchers have already begun injecting formulations into volunteers, others have begun testing vaccines on animals. Here's our guide to understanding the complex race for coronavirus vaccines.
Vaccines, also known as immunizations, are hailed by health experts as the single most powerful medical tool for improving the health of millions around the world. The WHO’s introduction of immunization programmes in 1974 have prevented hundreds of unnecessary child deaths around the world.
To understand how vaccines work, we need to understand how the immune system works. When a harmful virus or bacteria enters a body, they start to reproduce. The human body responds to these germs by identifying them as foreign invaders and making proteins known as antibodies. The primary task of these antibodies would be to destroy the germs that are making the body sick. Secondly, these antibodies would also try to protect you from any future infections. If the same germs invade your body a second time, the antibodies would come to your defence. When these antibodies are experienced in fighting these germs, they are able to destroy them before the germs have a chance of making you ill.
Vaccines help the body develop immunity by imitating an infection. A weakened form of a disease is injected to a person, so that the human body learns to produce antibodies. These vaccines are usually made of dead or weakened antigens, which can't cause an infection. The immune system however will still recognise these substances as an enemy invader and produce antibodies in response. As a result, the body would be well prepared to fight the same infection in future.
Several of the most feared diseases such as polio and smallpox which used to result in high death rates were nearly eradicated thanks to successful immunization campaigns around the world. Diseases such as measles, mumps and other epidemics too have been prevented from spreading due to immunization. Historically the smallpox vaccine is the only vaccine which has been able to completely eradicate a disease. However the smallpox vaccine has been far from pleasant to the body. It left a scar on the arm of those who received the vaccine and many have experienced severe discomfort and other side effects post vaccination.
According to the World Health Organisation's draft landscape of Covid-19 candidate vaccines published on June 16, there are 11 candidate vaccines in clinical evaluation, while another 128 candidate vaccines are in preclinical evaluation. Vaccines take a long time to be developed, licensed, and manufactured at a global scale. In normal times, rarely would a vaccine be approved in less than four to five years. But our times are not normal and the efforts to develop a vaccine are now global. If the coronavirus vaccine if successful, it is set to be the fastest developed vaccine in our history.
Bill Gates, an outspoken advocate for diligent medical research said that humans have never had a more urgent task than creating broad immunity for coronavirus. "Realistically, if we’re going to return to normal, we need to develop a safe, effective vaccine. We need to make billions of doses, we need to get them out to every part of the world, and we need all of this to happen as quickly as possible," Gates wrote in April. US public health expert Dr. Anthony Fauci meanwhile opines that a coronavirus vaccine may take as long as eighteen months to develop. Others suggest that it could take up to 9 months or even two years.
According to British scientific journal Nature, there are four main approaches to the vaccine, which are aimed at safely triggering a natural response to Covid-19.
Many existing vaccines are made in this way, such as those against measles and polio, but they require extensive safety testing. China’s Sinovac Biotech has tested an inactivated version of SARS-CoV-2 in humans and have announced positive results in phase I and II of clinical trials.
A virus such as measles or adenovirus is genetically engineered so that it can produce coronavirus proteins in the body. These viruses are weakened so they cannot cause disease. There are two types: those that can still replicate within cells and those that cannot because key genes have been disabled. Researchers at Oxford University and Johnson and Johnson are currently developing Covid-19 vaccines using this approach.
These vaccines aim to use genetic instructions (in the form of DNA or RNA) for a coronavirus protein that prompts an immune response. The nucleic acid is inserted into human cells, which then churn out copies of the virus protein; most of these vaccines encode the virus’s spike protein.
Many researchers want to inject coronavirus proteins directly into the body. Fragments of proteins or protein shells that mimic the coronavirus’s outer coat can also be used.
At least a dozen potential vaccines have now reached the human trial stage and some of them are reported to have promising results. Estimating the probability of success of a clinical trial is a daunting task. However the following candidate vaccines are the apparent frontrunners in the Covid-19 vaccine race. Most of these candidate vaccine companies are now looking at ramping up manufacturing ahead of approval, to ensure rapid distribution of doses if their candidate vaccine proves to be effective against the virus. China has five vaccine candidates for COVID-19 in human trials, the most in any country.
Oxford University's candidate vaccine, ChAdOx1 nCoV-19, a collaboration with British drugmaker AstraZeneca is an experimental vaccine which has garnered attention since trials began in April. The vaccine uses a weak mutation of the common cold virus (adenovirus) spiked with proteins from the novel coronavirus to build immunity. The vaccine is likely to offer protection against contracting Covid-19 for up to a year. It is currently in late-stage clinical trials in Britain, while trials have also been approved in the US and Brazil. The clinical trials are reported to involve a total of more than 10,000 people across the UK.
US Biotech company Moderna's RNA vaccine was the first to enter clinical trials and was touted as the frontrunner. Although the vaccine remains unapproved, the company has outlined phase 3 of their clinical trials set to begin in July. Moderna's first stage of the clinical trials for its vaccine named mRNA-1273, has reported promising positive results on at least 8 candidates who developed protective antibodies against coronavirus. While phase 2 is currently underway, phase 3 trials will focus on the vaccine's efficacy in preventing symptomatic Covid-19 disease and the prevention of severe cases of Covid-19.
China’s Sinovac Biotech this week announced that its coronavirus vaccine is safe and capable of drawing an immune response from its human trials. In a press release the company said that the vaccine hasn’t caused severe side effects, adding that more than 90% of the people administered the vaccine during a 14 day interval have induced neutralizing antibodies, two weeks after vaccination. Sinovac’s preliminary findings come from phase I and II trials conducted in China. The company also announced a partnership this month with Instituto Butantan, a Brazilian immunobiologic producer to conduct its phase III trial in Brazil, where the second-largest outbreak of coronavirus has erupted, killing more than 45,000 people.
Another frontrunner from China, CanSino Biologics Inc became the first vaccine to proceed to the second stage of the study and also to have its preliminary findings peer reviewed. Similar to Oxford's vaccine, this is the other viral vector vaccine which progressed into human trials in April. The vaccine was made with a certain mutation of a virus, named Ad5, which genetically modifies the protein structure when injected into a cell. According to the Beijing Institute of Biotechnology and other organizations the trials have shown promising results but need further research to demonstrate effectiveness against the virus.