Reply To:
Name - Reply Comment

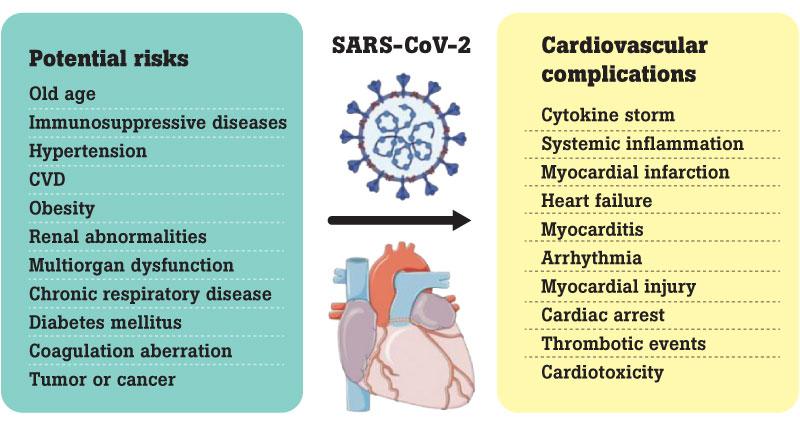
 cardiovascular diseases (CVDs) are the leading cause for global mortality; which is estimated at17.9 million lives per annum, according to the WHO. However, some clinical studies reveal that the global mortality rate by cardiac has been elevated significantly during this COVID 19 pandemic period and that COVID-19 can cause the cardiovascular disorders, including myocardial injury (death of cardiac muscle cells), arrhythmias (a problem with the rate or rhythm of the heartbeat), acute coronary syndrome (ACS) (due to suddenly reduced blood flow to the heart) and venous thromboembolism (VTE) (blood clot forms in a deep vein) due to a combination of the severe viral illness and its increased demands on the heart, increased heart rate compounded by low oxygen levels due to respiratory symptoms, myocarditis and increased propensity for blood clot formation. Some recent clinical studies show evidence of heart failure in COVID-19 patients even without pre-existent cardiovascular diseases. Moreover, Post-acute COVID-19 is a major concern for patients affected by cardiovascular disease
cardiovascular diseases (CVDs) are the leading cause for global mortality; which is estimated at17.9 million lives per annum, according to the WHO. However, some clinical studies reveal that the global mortality rate by cardiac has been elevated significantly during this COVID 19 pandemic period and that COVID-19 can cause the cardiovascular disorders, including myocardial injury (death of cardiac muscle cells), arrhythmias (a problem with the rate or rhythm of the heartbeat), acute coronary syndrome (ACS) (due to suddenly reduced blood flow to the heart) and venous thromboembolism (VTE) (blood clot forms in a deep vein) due to a combination of the severe viral illness and its increased demands on the heart, increased heart rate compounded by low oxygen levels due to respiratory symptoms, myocarditis and increased propensity for blood clot formation. Some recent clinical studies show evidence of heart failure in COVID-19 patients even without pre-existent cardiovascular diseases. Moreover, Post-acute COVID-19 is a major concern for patients affected by cardiovascular disease
The source person for today’s article is Dr.Lakshan Jayathilaka, Medical Officer, Base Hospital Karawanella.
Spectrum of Clinical Presentations
Heart failure in patients with COVID-19 may be precipitated by acute illness in patients with preexisting known or undiagnosed heart disease, acute hemodynamic stress, or acute myocardial injury. Cardiovascular risk factors and cardiovascular disease are highly prevalent in hospitalised patients with COVID-19. Patients with a known history of HF may suffer an acute decompensation due to the development of COVID-19 disease.
Right Heart failure is due to acute pulmonary hypertension precipitated by acute pulmonary embolism or adult respiratory distress syndrome (ARDS) has been described in patients with COVID-19. Venous thromboembolism (including extensive deep vein thrombosis and pulmonary embolism) is common in acutely ill patients with COVID-19.
Cardiac shock is a life-threatening condition in which your heart suddenly can’t pump enough blood to fulfill body’s needs.
According to the above mentioned facts there are several types of post-covid cardiac disease clinical presentations while some patients do not show symptoms. Therefore, rapid and accurate cardiovascular disease diagnosis is an essential factor to save the life of a person who has been experiencing post COVID conditions.
How to diagnose post COVID cardiac diseases
The various ECG findings observed in patients with COVID-19 likely reflect the combined effects of acute illness and chronic heart disease.
A variety of echocardiographic findings have been identified in patients with COVID-19
Cardiovascular magnetic resonance (CMR) abnormalities have been identified in patients with COVID-19 as well as in patients who have recently recovered from COVID-19.
Tropanin protein is the most commonly used biomarker in cardiac disease diagnosis since it has the highest known sensitivity. It enters into bloodstream soon after a heart attack. It also remains in bloodstream days after all other biomarkers go back to normal levels. Two forms of troponin may be measured: troponin T and troponin I. Troponin I is highly specific to the heart and stays higher longer than creatinine kinase-MB. Current guidelines from the American Heart Association (AHA) maintain that this is the best biomarker for finding a heart attack.
This enzyme can also be measured several times over a 24-hour period. It will often at least double if you’ve had a heart attack. Since levels of CK can go up in many other conditions besides a heart attack, it is not very specific.
This is a subtype of CK. It is more sensitive when detecting heart damage from a heart attack. CK-MB rises 4 to 6 hours after a heart attack and generally returns to normal in a day or two. Because of this, it’s not helpful when a healthcare provider is trying to figure out if your recent chest pain was caused by a heart attack.
 Myoglobin
MyoglobinThis is a small protein that stores oxygen. It is measured occasionally. Myoglobin is sometimes measured in addition to troponin to help diagnose a heart attack. It is also not very specific for finding a heart attack.
High sensitive C-reactive protein (hs-CRP) is a highly sensitive cardiac biomarker which can be used as an independent risk factor for predicting adverse cardiovascular diseases. As mentioned in a number of research studies, an increase in serum hs-CRP could be seen in patients with acute myocardial injury. This information is vital if you are also infected with COVID 19 virus and have this post covid condition with cardiac disease.