Reply To:
Name - Reply Comment

 All human beings at a certain point in their lives have experienced a disease affecting them or their loved ones. Be it in the form of your run-of-the-mill cold to more complex incurable terminal afflictions like cancer, the common ground that all these ailments share is ‘pain and suffering.’
All human beings at a certain point in their lives have experienced a disease affecting them or their loved ones. Be it in the form of your run-of-the-mill cold to more complex incurable terminal afflictions like cancer, the common ground that all these ailments share is ‘pain and suffering.’
Although pain can be resolved for the most part by adequate pain killers or analgesia the aspect of ‘suffering’ and how it affects an individual is rarely addressed.
This is where Palliative Care plays an integral role in the modern health care setup. Palliative Care as defined by the World Health Organization (WHO) is ‘an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and assessment and treatment of pain and other problems which are physical, psychosocial and spiritual.’ It is estimated roughly that over 40 million incurably ill and dying people require Palliative Care annually. And a vast majority does not have access to the facilities they desperately require.
The modern concept of Palliative Care was first introduced by a British Anglican physician named Dame Cecily Saunders, who emphasised the importance of Palliative Care in modern medicine. She also played an integral role in establishing the first contemporary hospice in 1967 which was St.
Christopher’s Hospice in South London. The word ‘palliative’ is derived from the Latin word palliare which means ‘to cloak.’ Palliative care is usually provided by Palliative Care specialists – health care professionals who have received specialized training or are certified in providing palliative care. This field requires a multidisciplinary team-which comprises of doctors, nurses, physiotherapists, psychological counselors, certified dieticians, alternative medical therapists (e.g. acupuncturist) caregivers, priests and social workers-in order to make it effective. The objective of this ‘team’ is to improve the overall Quality of Life of the patient. All human beings are endowed with the need to communicate- to talk, be listened to and to feel relevant-and patients treated through Palliative Care are no different. Some individuals who receive a terminal diagnosis tend to find solace in their religious or spiritual believes whilst others tend to question their beliefs and ask ‘why they are in this current predicament.’ When bad news is broken to a patient the emotional changes the affected individual and caregivers endure cannot be summed up in words, but it affects all, in a detrimental manner. The patient may feel the need to isolate themselves from society due to the stigmatizing effect of the disease or due to loss of their jobs/social status following the diagnosis of the affliction. Therefore, engaging in active listening and participating in empathic conversations-involving patient and caregiver alike-plays a pivotal role in changing the mindset of an individual. Altering the sufferers’ outlook to a more positive one almost has a therapeutic effect on them, even alleviating their pain.
The modern concept of Palliative Care was first introduced by a British Anglican physician named Dame Cecily Saunders, who emphasised the importance of Palliative Care in modern medicine
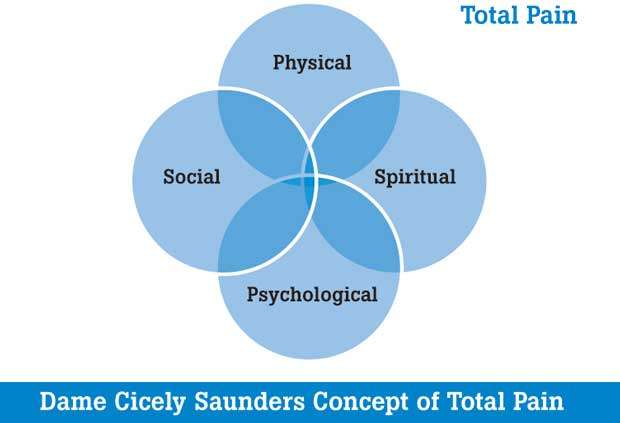
Pain management also plays an important role in the process of Palliative Care. Dame Cecily Saunders promulgated that the ‘Total Pain’ endured by an individual includes various aspects such as physical, psychological, spiritual and social. Alleviation of pain successfully is, therefore a holistic process whereby all these aspects must be addressed according to her. The International Association for Study of Pain defines pain as ‘An unpleasant sensory and emotional experience associated with actual or potential tissue damage.’ For all practical purposes though ‘pain’ is when a person says “it hurts” since it is a subjective phenomenon. Depending on the duration of pain it is customarily classified into acute and chronic; whereas an Acute Pain is defined as a pain lasting less than three 3 months duration a Chronic Pain exceeds 3 months. But it’s concerning the latter form of pain that Palliative Care is primarily concerned with. Chronic Pain is one of the most significant causes of prolonged suffering and disability worldwide concerning both communicable (e.g. HIV/AIDS) and non-communicable diseases (e.g. cancer and diabetes mellitus) Whilst Acute Pain serves a biological function by decreasing potential damage to the body, Chronic Pain is not known to serve such a purpose. It differs vastly from Acute Pain in terms of presentation as well; with symptoms ranging from sleep disturbance, mood changes and restriction of social activities.
Many patients enduring insufficient pain relief may seek more expensive alternative modes and this may also cause a major financial burden to the family or caregiver of the patient. The management of Pain in the hospital setup is done according to the WHO analgesic ladder usually in a step-wise manner. The first step of the ladder comprises of non-opioid analgesics such as aspirin, paracetamol and Non-Steroidal Anti-Inflammatory drug (NSAIDS) such as diclofenac sodium. Step 2 and 3 mainly includes the addition of opioid analgesics to step 1 (weak opioids such as codeine/tramadol in step 2 and strong opioids like morphine in step 3). Broadly speaking opioids are a group of drugs that act on the central nervous system to relieve pain. But abuse of them can lead to withdrawal and physical dependence. When one observes the current trend of Disease Burden across the world it is abundantly obvious that there has been a sharp increase in both communicable and non-communicable diseases. The role that Palliative Care plays in both is an integral one. As such the need to address this need and integrating Palliative Care to the health care systems the world over is both a timely and important one.
(The writer is a
MO - Dialysis Base Hospital , Telliapallei)