Reply To:
Name - Reply Comment

 After a rainy season, most of the time, a dengue epidemic would start since it allows the increase of mosquito breeding places. Dengue is a mosquito born disease which is caused by flavivirus namely, Aedes mosquito which affects a large number of people. Individuals are mainly affected in tropical and sub-tropical regions in the world causing a significant morbidity and mortality. After this monsoon period we have to protect ourselves from the dengue virus by avoiding mosquito spreading and taking sufficient health management precautions before it manifests to a severe stages of dengue infection such as Dengue Hemorrhagic Fever and Shock Syndrome. That is why Health Capsule has selected this topic for discussion this week.
After a rainy season, most of the time, a dengue epidemic would start since it allows the increase of mosquito breeding places. Dengue is a mosquito born disease which is caused by flavivirus namely, Aedes mosquito which affects a large number of people. Individuals are mainly affected in tropical and sub-tropical regions in the world causing a significant morbidity and mortality. After this monsoon period we have to protect ourselves from the dengue virus by avoiding mosquito spreading and taking sufficient health management precautions before it manifests to a severe stages of dengue infection such as Dengue Hemorrhagic Fever and Shock Syndrome. That is why Health Capsule has selected this topic for discussion this week.
According to research studies dengue serotype 3 is affecting the people of Sri Lanka this year. As mentioned by the Epidemiology Unit of the Ministry of Health, 38,180 people have been infected by the dengue virus covering a period between January to mid August.
Transmission
The vector for dengue, Aedes mosquito, bites during the day time. However, the highest biting intensity is about two hours after sunrise and before sunset. The infected Aedes mosquito bites 4-5 people at a time which results in multiple dengue cases in the same area.
The period of transmission from humans to mosquitoes begins one day before the start of fever up to the sixth day of illness corresponding to the viremia phase - the stage at which the virus will be present in the blood stream. After a female mosquito bites an individual in the viremia phase, viral replication begins in the vector in from eight to twelve days. In humans, the incubation period ranges from 3 to 15 days (intrinsic incubation) with an average of 5 days.
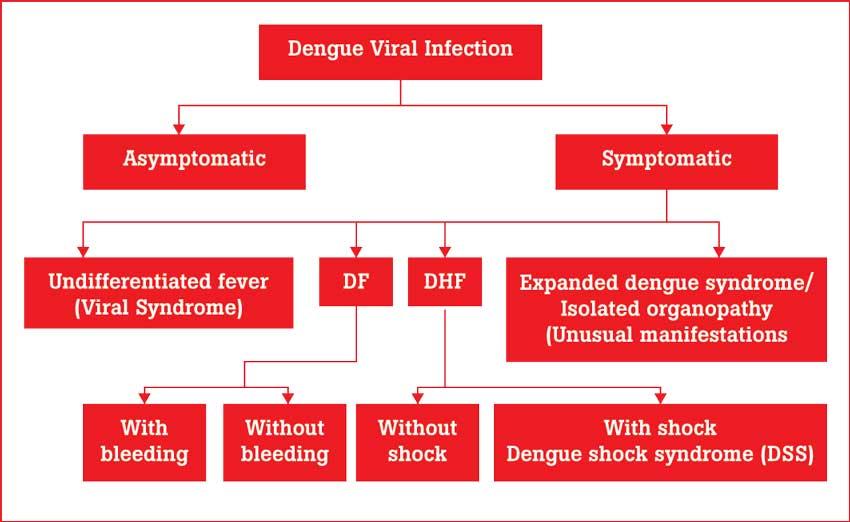
Dengue Classification
Undifferentiated fever
Those who have been infected with the dengue virus, especially for the first time (i.e. primary dengue infection), may develop a simple fever, indistinguishable from other viral infections.
Dengue fever (DF)
It is generally an acute febrile illness, with some symptoms such as severe headache, pain in muscles and joints and rashes. Leucopenia (reduction in the number of white cells in the blood) and thrombocytopenia (deficiency of platelets in the blood) may also be observed. Although DF may be benign, it could be an incapacitating disease with severe headache, muscle and joint and bone pains (Breakbone Fever).
Occasionally unusual haemorrhage such as gastrointestinal bleeding, hypermenorrhea and massive epistaxis may also occur.
Dengue Haemorrhagic Fever (DHF)
DHF is characterised by the acute onset of high fever and is associated with signs and symptoms similar to DF in the early febrile phase. Plasma leakage is the hallmark of DHF which occurs soon after the end of the febrile phase. There is a tendency to develop hypovolemic shock (dengue shock syndrome) due to plasma leakage.
Diagnosis
Dengue has significant health, economic and social impacts on affected communities. Prompt case detection and the implementation of appropriate clinical management are required to reduce the mortality from severe dengue since there is no vaccine or specific antiviral therapy at present to address the growing threat of dengue. In practice, disease diagnosis for Dengue is often made by clinical signs and symptoms only. Hence, laboratory confirmation of the dengue virus infection is important. Sometimes, dengue can also be confused clinically with other vector-borne viral and parasitic diseases, such as malaria and chikungunya and zika viruses. Therefore sudden disease progression from an acute phase to chronic phase and even mortality can result from these misleading clinical confirmations. Therefore, implementing timely, appropriate clinical management, which involves early clinical and laboratory diagnosis is required to reduce mortality from the dengue infection. The presence of antigen and antibodies changes as the days progress with the illness. Normally antigens retain in blood only for the first 4 days and therefore the NS1 dengue antigen test is valid only for 4 days while the dengue antibody test is valid after 4th day of illness to the 9th day since dengue antibodies namely Ig G and Ig M retain in blood for few days after the infection.
Clinical signs of dengue Muscle pain
Dengue is associated with many neurological dysfunctions. According to research studies, up to 4% of dengue patients may develop neuromuscular complications. Muscle pain is the most characteristic neurological symptom of dengue fever noted during the early phase of the illness. Muscle pain commonly affects the back and proximal limb muscles. Patients may experience difficulty in walking because of muscle pain. Distributed viral invasion of muscles and subsequent inflammatory changes in the muscles result in muscle pain due to the dengue virus thus affecting the muscle satellite cells which are responsible for muscle repair after injury. The Dengue virus infection has also been found to impair the ability of the dengue virus -infected muscle satellite cells to up-regulate myosin heavy chain I protein levels, suggesting that an immune mechanism may be responsible for the muscle damage.
High fever and headaches
The hypothalamus controls body temperature, which usually varies throughout the day. In the case of dengue infection, hypothalamus may reset the body to a higher temperature.
Skin rashes
Many of the studies have reported that skin dendritic cells are likely the initial target of DENV infection in humans. The pathogenesis of skin rash can be caused by the interaction between the virus and host cells, which subsequently leads to release of different types of chemical mediators and initiation of the immunological mechanisms.
Pain behind the eye
The onset of visual symptoms occurs on or close to the day of the lowest serum platelet level which results in a bleeding tendency, which gives rise to increased incidence of haemorrhage. These haemorrhages manifest as retinal blot haemorrhages in the macula (the central area of the retina) and retinal periphery.
Nausea and vomiting
Fatigue
The fatigue is defined as a collection of symptoms, mainly from muscular and neurological origin. The pathogenesis of dengue fatigue is likely multifactorial and could result from a combination of pathogenic effects produced by the virus and the immune response of the host to the dengue virus due to certain types of infections, toxic substances released from the body and accumulated in the brain causing fatigue.
Mild bleeding
Mild haemorrhagic manifestations might be due to increased capillary insubstantiality as a result of thrombocytopenia (low platelets count) or platelet dysfunction. Normally, platelets release factors that help maintain the integrity of the endothelial adherence junctions. Major mucosal bleeding (gastrointestinal or vaginal) in dengue patients can be occult and is often associated with prolonged shock and metabolic acidosis( imbalance chemical composition of acid and base in our blood )
Haematological dynamics
Leucopenia- Low leukocyte count in dengue infection may be due to virus induced inhibition/destruction of myeloid progenitor cells which are precursors of red blood cells, platelets, granulocytes such as neutrophils, eosinophil, basophils, monocyte-macrophages, dendritic cells, mast cells and osteoclasts.
Neutropenia- Dengue is a virus disease therefore there should have higher lymphocytes count. However, Neutropenia is one of the most significant clinical findings in dengue patients, suggesting that neutrophils have a crucial role in the pathogenesis of dengue virus infection.
Polymorphonuclear neutrophils are the most abundant white blood cells in the blood and constitute the first line of host defense against numerous infectious pathogens, including bacteria, fungi, and protozoa. Neutrophils are the first leukocytes to migrate to sites of inflammation and infection where they recognise and phagocytose invading microorganisms, in order to kill them via different cytotoxic mechanisms. This process involves molecular mechanisms that coordinate cell polarization, delivery of receptors, and activation of integrin at the leading edge of neutrophils migrating toward chemo attractant. Once at sites of infection, neutrophils actively phagocytose microorganisms or form neutrophil extra cellular traps (NETs) to trap and kill pathogens.
Thrombocytopenia
A low platelets count is known as thrombocytopenia. Platelets play a basic role in the process of haemostasis (preventing bleeding from damaged blood vessel). The Dengue virus induces the bone marrow suppression. Since bone marrow is the manufacturing centre of blood cells its suppression causes deficiency of blood cells leading to low platelet count. Moreover, research studies suggest that dengue virus can even bind to platelets of human blood in the presence of virus-specific antibodies and the antibodies that are produced after infection of dengue virus can contribute in destruction of platelets, thus lowering the platelet count. Furthermore, when vascular endothelial cells that are infected with dengue virus gets combined with platelets they tend to destroy platelets and this is one of the major causes of low platelet count in dengue fever.
Haemoglobin
In DHF patients there is an increased vascular permeability that gives rise to loss of plasma from the vascular compartment into the extravascular tissue. This would result in an increased concentration of haemoglobin concentration in the blood vessel. These significant changes of vascular permeability leads to the alteration function in the cellular membrane in maintaining the fluid osmotic pressure and ion concentration gradient between the intracellular and extracellular compartments. This mechanism affects the reactance and indirectly reflects an increased concentration of hemoglobin.
High haematocrit value
The increase in haematocrit in dengue is due to haemoconcentration attributed to plasma leakage induced by cytokine-mediated increase in vascular permeability and damage to vascular endothelium. Cytokines are responsible to produce DENV infected monocytes, B lymphocytes and mast cells. Endothelial cell dysfunction by virus also leads to increased capillary permeability. This phase of plasma leakage is the critical phase, the onset of which can be predicted with the rise of haematocrit 10–15% above the baseline value.
Biochemical dynamics
Increase liver enzymes
Hepatic dysfunction is a critical feature seen in DENV infection since Hepatocytes and Kupffer cells are prime targets for DENV infection. Liver enzymes especially aspartate aminotransferase (AST or SGOT) and alanine aminotransferase (ALT or SGPT) elevation are common in dengue since these enzymes are indicators of liver injury. Usually the SGOT levels are more than SGPT levels probably due to skeletal muscle injury while research studies have noted that the average levels of AST and ALT were significantly higher in DHF patients than in DF due to severe liver damage by fluid leakage, oxidative stress or immune mediated injury occur in DHF patients.
Why fluid balance is important?
The clinical course of dengue includes febrile, critical and recovery phases and there are different challenges for fluid management at each stage. During the critical stage, an increase in capillary permeability and shock can result if a large volume of plasma is lost through leakage. The recommended regimen for the treatment of DSS is immediate and rapid replacement of the plasma loss with isotonic crystalloid solutions such as saline or, in the case of profound shock, colloid solutions and continued replacement of further plasma losses to maintain effective circulation for 24–48 hours. Correction of metabolic and electrolyte disturbances and blood transfusion is done in cases with severe bleeding. If large amounts of fluid are required, these should be reduced gradually as plasma leakage decreases in order to prevent fluid overload, an excess in plasma volume which can cause oedema (abnormal accumulation of fluid in certain tissues within the body), respiratory distress or congestive heart failure, during the recovery stage.
Conclusion
Dengue is a critical health problem in our country. However, still no one has found proper treatment for this infection since the dengue virus is a very rigid one and there are four dengue serotypes (DENV1, DENV2, DENV3 and DENV4). However, once a person is vulnerable to the dengue infection, that person gets lifelong immunity to that particular serotype and as discovered in researches that previously dengue infected people will also not get the other three (DENV2, DENV3 and DENV4).
The writer is a medical laboratory technologist at a private hospital and holds a MSc. Degree in Industrial and Environmental Chemistry from the University of Kelaniya and a BSc in Food Production and Technology Management degree from the Wayamba University of Sri Lanka.