Reply To:
Name - Reply Comment

 As more cases of the Omicron variant are being detected in Sri Lanka, health authorities are taking maximum efforts to prevent another wave from interfering with the day-to-day lives of people. Initially detected in early December, the Omicron variant (B 1.1.529) is said to be having 50 gene mutations while 32 of them are in the spike protein and 15 within the receptor binding domain. The variant was initially discovered in South Africa where in November around 400 cases were reported and this figure jumped to about 6000 during the early part of December. With only preliminary research available, health experts are trying to study the nature of the variant and how effective the available treatments and vaccines would be.
As more cases of the Omicron variant are being detected in Sri Lanka, health authorities are taking maximum efforts to prevent another wave from interfering with the day-to-day lives of people. Initially detected in early December, the Omicron variant (B 1.1.529) is said to be having 50 gene mutations while 32 of them are in the spike protein and 15 within the receptor binding domain. The variant was initially discovered in South Africa where in November around 400 cases were reported and this figure jumped to about 6000 during the early part of December. With only preliminary research available, health experts are trying to study the nature of the variant and how effective the available treatments and vaccines would be.
Monoclonal antibodies and convalescent plasma
“Antivirals are based on basic knowledge about viral genome and what it encodes,” opined Prof. Dushyantha Jayaweera, Professor in clinical medicine at University of Miami Miller School of Medicine at a recently concluded discussion organised by the Sri Lanka Foundation. “All drugs that are working are based on genes that are encoded, this could be RNA dependent RNA Polymerase or the spike protein, membranes or the envelope. As such, drug development has been based on what genes do we target and how do we interrupt the life cycle so that these structural proteins are disrupted,” said Prof. Jayaweera.
 “Monoclonal antibodies are commonly used in States. Casirivimab and Imdevimab and a single mAb (sotrovimab) have shown to reduce the risk of hospitalization and death in the outpatient setting in those with mild to moderate COVID-19 symptoms. Currently the monoclonals have in-vitro susceptibility against variants, at least for Delta. With regards to monoclonal antibodies we start within 10 days of symptom onset and if you take them, the vaccination has to be delayed by 90 days as a precautionary measure since antibody treatment may interfere with vaccine-induced responses,” the professor added.
“Monoclonal antibodies are commonly used in States. Casirivimab and Imdevimab and a single mAb (sotrovimab) have shown to reduce the risk of hospitalization and death in the outpatient setting in those with mild to moderate COVID-19 symptoms. Currently the monoclonals have in-vitro susceptibility against variants, at least for Delta. With regards to monoclonal antibodies we start within 10 days of symptom onset and if you take them, the vaccination has to be delayed by 90 days as a precautionary measure since antibody treatment may interfere with vaccine-induced responses,” the professor added.
Shedding light on Omicron, Prof. Jayaweera further said that it has multiple mutations in the receptor-binding domain and other sites which leads to enhanced transmissibility. “It also has an ability to evade innate immunity. By doing all that it increases infectivity. One of the findings is that when it comes to Omicron, none of these monoclonal antibodies will work. There’s also data to show how badly the vaccines are working against this variant. Some vaccines show a 100-fold reduction in efficacy,” explained Prof. Jayaweera.
In conclusion he spoke about COVID Convalescent plasma and it’s importance in the case of Omicron. “If you take plasma from the same area with a high titer and if you give it at the onset of disease, then it works. If vaccines don’t work then consider COVID convalescent plasma in Sri Lanka because it’s easy to get the plasma and use it and it is much cheaper than other methods.” the professor said.
In conclusion he said that vaccines may not work against Omicron variant but that it’s the best way to protect against the virus.
Infectivity and transmissibility of Omicron
Adding her comments, Prof. Neelika Malavige, Professor at Department of Immunology and Molecular Medicine, University of Sri Jayawardenapura said that countries such as USA, Canada, South African region, India has shown community transmission of Omicron. “In Sri Lanka Omicron was detected in a traveller but from recent  sequencing data we now know that it’s not just present in travellers but it has been detected from people in the community, who had links with travellers. When it comes to transmissibility – South Africa initially reported it on November 24 – and within a matter of two days the WHO declared it as a Variant of Concern (VoC). But in the case of other variants the WHO took few weeks to declare them as potential VoCs. What is worrying about Omicron is high transmissibility and infection rate.” added Prof. Prof. Malavige.
sequencing data we now know that it’s not just present in travellers but it has been detected from people in the community, who had links with travellers. When it comes to transmissibility – South Africa initially reported it on November 24 – and within a matter of two days the WHO declared it as a Variant of Concern (VoC). But in the case of other variants the WHO took few weeks to declare them as potential VoCs. What is worrying about Omicron is high transmissibility and infection rate.” added Prof. Prof. Malavige.
She further said that UK is currently facing a huge surge of COVID cases and in certain areas such as London, Omicron has displaced Delta. “When it comes to viruses it’s about survival of the fittest. We know that when the Delta variant emerged it wiped out all other variants and it was the predominant variant globally for quite a long time. But now, Omicron is more transmissible than Delta and is therefore wiping out the Delta variant. In Sri Lanka, 1% of our sequencing is Omicron but it will change a little bit.
“Omicron also has a potential to cause reinfection,” she added. “Even with earlier variants they did cause reinfections in people who had natural infections but because of mutations in Omicron, especially in sites where neutralizing antibodies bind, there’s a higher immune escape associated with Omicron. As such the relative risk of reinfection for Omicron is 25% when compared to Beta which had a 12% relative risk of reinfection while Delta stood at 9% .
“Infectivity depends on where Omicron can infect. A Hong Kong university study showed that it can cause 70 times more infectivity when in upper airways where the virus can be disseminated out rather than lower airways. This can reduce infection in the lung which can lead to less severe disease but more infection in the bronchus can lead to more infection rate. It is also said that the transmission rate of Omicron is also similar to measles which is one of the highest transmissible virus we have seen.”
“Most monoclonal antibodies don’t seem to be working for Omicron but we have vaccines. Sri Lanka has ordered doses for every adult in the county and it’s important at this moment to get your booster dose and get as much protection as possible,” she advised in her concluding remarks” said Prof. Neelika Malavige.
To be boosted or not to be boosted ?
Speaking about vaccine effectiveness against Omicron Prof. Suranjith Seneviratne, Consultant in clinical immunology and allergy, Institute of Immunity Transplantation and Health Services Laboratories, London, UK said that the spike protein binds to the ACE2 receptor. “It divides and multiplies within the cell, spreading from cell to cell and person to person. We are concentrating on spike protein because most vaccines directed towards spike protein – so any changes in spike protein will have a potential effect on vaccine escape,” Prof. Seneviratne.
 He described Omicron as a very different virus to what was originally found in Wuhan. Speaking about administering vaccines, he said that an immunocompromised patient would go for a third dose which is equivalent to two doses on a patient who has a normal immune system. “The booster is the third dose for a person with a normal immune system and the fourth dose for a person with an impaired immune system.
He described Omicron as a very different virus to what was originally found in Wuhan. Speaking about administering vaccines, he said that an immunocompromised patient would go for a third dose which is equivalent to two doses on a patient who has a normal immune system. “The booster is the third dose for a person with a normal immune system and the fourth dose for a person with an impaired immune system.
“With the booster the number of cases in Israel for instance started reducing which in turn reduced hospitalizations, disease severity and deaths. Therefore boosters are effective and safe and have been rolled out in many countries but equity of roll out isn’t great and that needs to be considered.” said Prof. Seneviratne.
He then shed light on several research studies and how it showed varying rates of neutralization against those who have had two jabs and a booster. In some studies neutralization reduced while in other the effectiveness was improved following a booster dose.
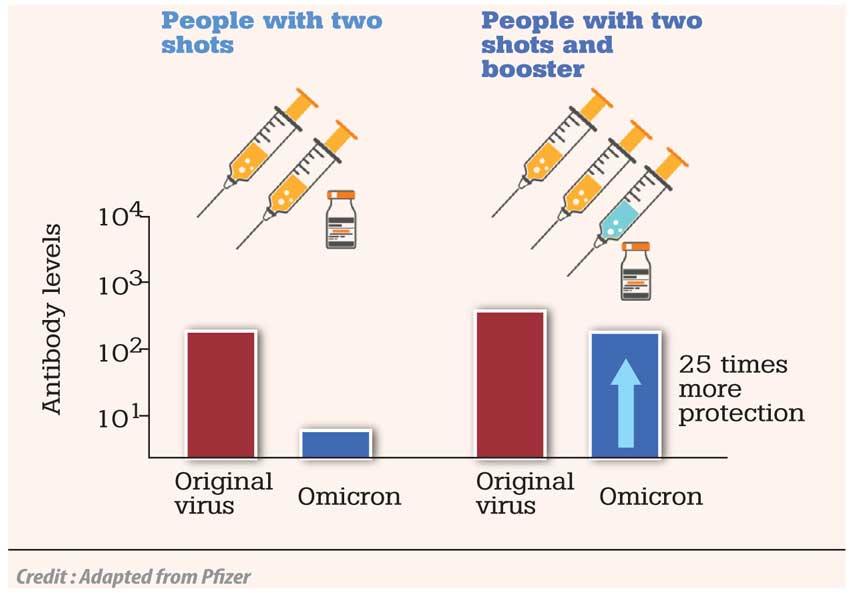
“The priority now is to increase vaccine uptake - the first thing is to get first two doses and then look at other doses as that would increase neutralization titers and have a positive effect on patients. But a study from Germany showed that even with a booster there was a small group of patients who had been infected with Omicron and this may give rise to the necessity of Omicron-specific vaccines but at the moment standard vaccines against older variants are working. If by chance there’s an increased amount of escape, then Omicron-specific vaccines may have to be developed. Already, vaccine manufacturing companies are working on that and have said that by March they would get a vaccine for regulatory authorities to be approved. But at the moment, it is the standard vaccines with a booster that’s found to increase the neutralization capacity,” concluded Prof. Seneviratne.