Epilepsy is one of the most common neurological diseases that has affected over 50 million people globally. While it is a chronic non-communicable disease it has been estimated that 70% of people could live seizure-free if properly diagnosed and treated. Epilepsy is also associated with a lot of stigma as people, especially those who are not trained in first aid, would react to it differently, often making the patient feel uncomfortable. During a discussion held recently to shed more light on its lesser known areas, Dr. Padma Gunarathne, Consultant neurophysician and President of Sri Lanka Association for Geriatric Medicine emphasised on the need to be aware of symptoms and triggers leading to a fit.
“We have learnt about electrical activity in the brain when you’re awake, when you’re asleep, how it is in the front and back of the brain, how it varies in children and adults, what changes happen when you become anxious etc. If there’s a sudden change based on many reasons you get a set of symptoms for a transient period. That set of symptoms is described as a fit. If it originates from one place we call it a focal fit. If it originates from both sides of the brain simultaneously all over the brain we call it a generalised fit,” she explained.
Who is an epileptic?
A fit could happen for so many reasons. “If someone has a tendency to get more fits with no particular reason we call that person an epileptic,” she added. “A characteristic feature of epilepsy is that it is transient, tends to happen for no reason and an attack that happens to a person happens for the same reason. So if he has a tumour and if it is the reason for the fit, then the symptoms that appear is the same for each and every fit. But there are varying types of fit,” she added.
Speaking on those who could be more prone to it, Dr. Gunarathne said that if there’s a delay in breathing at birth probably due to a damage to the brain, the child may develop a fit later in life. “It could also happen due to an infection to the brain, toxicity of alcohol or if you suddenly withdraw from alcohol. It could happen due to a head injury and is common in children. But adults could also have epilepsy due to a stroke or tumour,” said Dr. Gunarathne.
Symptoms and triggers
Generalized chronic -tonic seizure
Dr. Gunarathne said that during a generalised fit what is known to that person is that they would experience an aura before a fall. Some other symptoms include :
- blurry vision
- getting an odd feeling about the surrounding
- losing consciousness
- eyes, mouth and neck gone to a side
- making a loud cry before the fall
“Thereafter the person would have a stiff face (chronic face), patient would develop jerking of mouth, eyes and lips and within that period he may injure himself from the fall,” she added. “In the tonic phase, he would bite his tongue and eventually there would be froth coming out. This would last for about 30s and would be followed by another one or two minute period where he would be in deep sleep and the whole attack would last about 4-5 minutes. This is followed by the postictal phase where the patient could be confused. He would wake up and during that period one might be aggressive and be violent and would remain for about 10-15 minutes before the patient regains consciousness. Then he would have aches and pains or may vomit and for another 24 hours he would fall asleep while experiencing aches and pains. This is known as a generalised chronic -tonic seizure,” she said.
Absence seizure
There are many other varieties of fit. An absence seizure is where a children between 3-15 years with normal behaviour would suddenly experience a blank spell. “He might drop what is in his hands and this will last for about 20s. These attacks may happen every now and then and would have a disturbance in his school work. One may get about 100-200 attacks per day. There’s no area of the brain that this particular type of fit originates from,” said the doctor.
Myoclonous seizure
A third type of fit is called myoclonous seizure which have many varieties. “A particular variety is seen among teenagers with normal behaviour and normal intelligence. “If they are sleep deprived and wakes up the next day, they would experience a jerk. This would be one or several jerks. They may either drop something or they themselves would drop on the floor. It would be followed by a generalized chronic-tonic seizure,” said Dr. Gunarathne.
Focal fit
According to Dr. Gunarathne in this type of a fit, there is a focus or basically an area of the brain that discharges abnormal electrical impulses. This could be a tumour, head injury, or it could be that a patient had a stroke or an injured area of the brain. In some of the attacks those abnormal attacks are confined to the particular region where as in other attacks that abnormal electrical impulse could be generalised and may spread all over the brain. In this situation, the person would experience lip smacking, drooling of saliva, lost consciousness but the person may not fall to the ground and the attack would last for about 3 minutes.
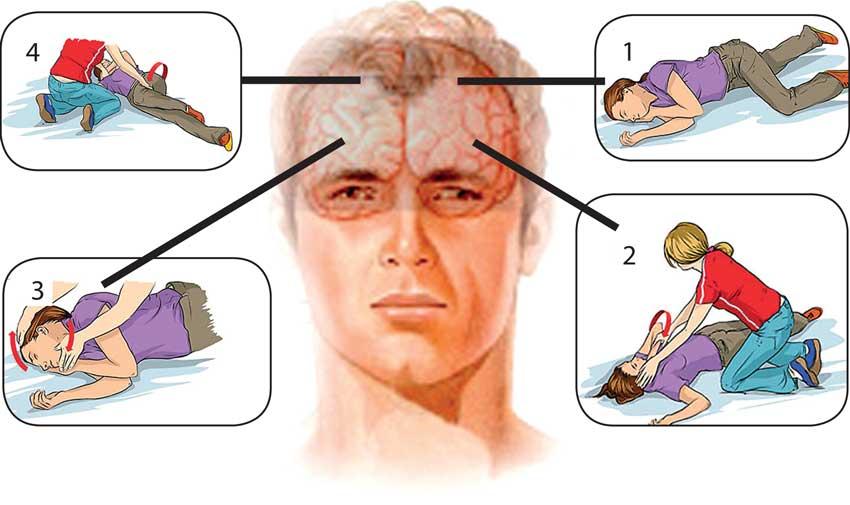
However Dr. Gunarathne said that epilepsy could be controlled in 95% of the cases except for 2-3% that may require surgical treatment. “Many fits could be controlled with drugs and what is important is adherence to drugs. It’s important that we all be able to recognise a fit. You could remove the person from a risky situation such as if you see the person drowning or during a fire. the person is in a place which is threatening such as drowning or fire, so you need to remove him. You could turn the person to the side so that you avoid the tongue falling and blocking the airway. Then hold the person and wait. Relatives know for how long it would last. Myths are that you should put the key to the mouth, give an iron rod, give the finger to the mouth etc,” he said.
Impact on mental health
Reflecting on the communal environment of Sri Lanka, behavioural health researcher, lecturer, Mental Health and Psychosocial Support (MHPSS) practitioner and co-Founder of Ohana Project Nilushka Perera said that people say a lot of things when you have an illness. “But we have to be aware when dealing with a chronic illness as many side effects could affect your mental health. Social influences have a bugger impact. Therefore, how your friends and family say and react to your condition may have an impact on your compliance with drugs. These factors should be considered at a diagnostic stage. If you look at the mental health impact it is confidence and self esteem that one may not have because epilepsy is an unpredictable condition. You don’t know when you would get an attack, be it a fit or anything, so you are scared to go to school or to a party and especially to work. If you’re not trained in first aid and if haven’t seen an epileptic person you will get scared and leave. Somas a community we could learn first aid and help that person. This is how the family and friends could make the patient feel comfortable in the surrounding. Because of the stigma people will not get diagnosed and if they are not diagnosed they will not disclose it. It’s a huge burden to carry alone. Epilepsy is a chronic illness people don’t want to talk about. So the mental health impact is more social with pressure coming from outside while you’re dealing and living with a chronic illness. Once diagnosed you could start lifestyle modifications, it will influence how others see you and how you ultimately deal with the illness,” said Perera.
“We are not comfortable about our emotions but our aches and pains,” said Perera. she added. “In most Asian countries we don’t know how to express our sadness. In English we know the terms to describe our emotions but colloquially there are less terms to describe our emotions in Sinhala and Tamil. Take the burden off your shoulders by voicing out your concerns and learn to articulate it to another person and give them the knowledge and resources about preparation. The public should be trained in first aid. An epileptic patient could injure himself from a fall and it could be prevented if people around him are trained in first aid. It is also advisable to have an emergency contact card in your wallet so that people would know whom to contact. People are going to react to you differently and that’s part and parcel of a person with a chronic illness”.
 Epilepsy is one of the most common neurological diseases that has affected over 50 million people globally. While it is a chronic non-communicable disease it has been estimated that 70% of people could live seizure-free if properly diagnosed and treated. Epilepsy is also associated with a lot of stigma as people, especially those who are not trained in first aid, would react to it differently, often making the patient feel uncomfortable. During a discussion held recently to shed more light on its lesser known areas, Dr. Padma Gunarathne, Consultant neurophysician and President of Sri Lanka Association for Geriatric Medicine emphasised on the need to be aware of symptoms and triggers leading to a fit.
Epilepsy is one of the most common neurological diseases that has affected over 50 million people globally. While it is a chronic non-communicable disease it has been estimated that 70% of people could live seizure-free if properly diagnosed and treated. Epilepsy is also associated with a lot of stigma as people, especially those who are not trained in first aid, would react to it differently, often making the patient feel uncomfortable. During a discussion held recently to shed more light on its lesser known areas, Dr. Padma Gunarathne, Consultant neurophysician and President of Sri Lanka Association for Geriatric Medicine emphasised on the need to be aware of symptoms and triggers leading to a fit.