Reply To:
Name - Reply Comment
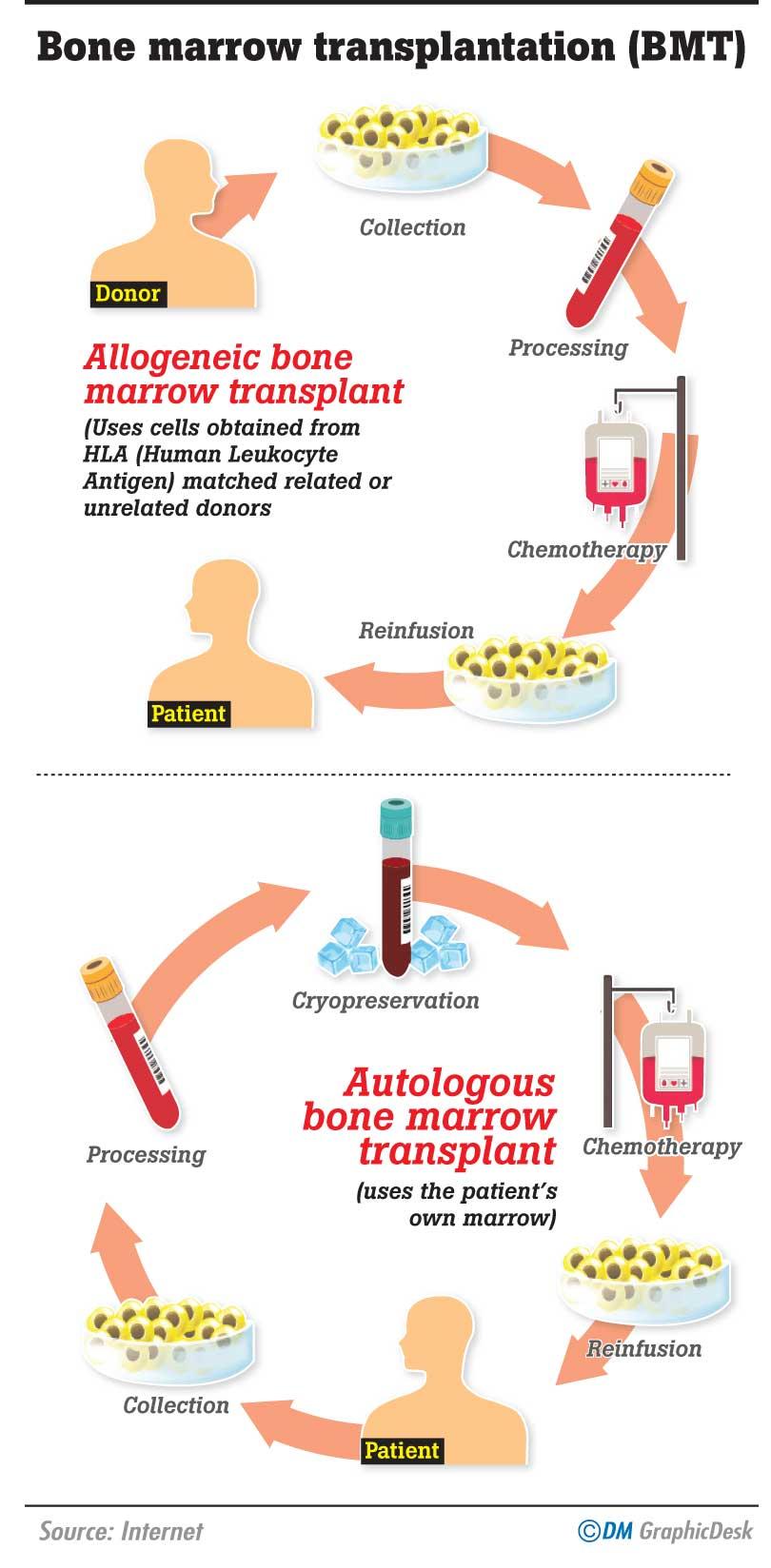
 Bone Marrow Transplantation (BMT) is a procedure where Transplant clinicians replace bone marrow that is diseased (or damaged) with healthy bone marrow. There are two main types of BMT namely; autologous and allogeneic. Autologous transplantation uses the patient’s own marrow and Allogeneic transplantation uses cells obtained from HLA (Human Leukocyte Antigen) matched related or unrelated donors. Leukaemia, Thalassaemia, Sickel-cell anaemia, Multiple Myeloma, Solid Tumours, Hodgkin’s Disease, Aplasticanaemia and primary immune deficiencies are just a few of the lengthy list of diseases in Sri Lanka for which Bone Marrow Transplantation would equal to life saving. However, due to the absence of a National Bone Marrow Donor Registry, the options are limited in the field of BMT.
Bone Marrow Transplantation (BMT) is a procedure where Transplant clinicians replace bone marrow that is diseased (or damaged) with healthy bone marrow. There are two main types of BMT namely; autologous and allogeneic. Autologous transplantation uses the patient’s own marrow and Allogeneic transplantation uses cells obtained from HLA (Human Leukocyte Antigen) matched related or unrelated donors. Leukaemia, Thalassaemia, Sickel-cell anaemia, Multiple Myeloma, Solid Tumours, Hodgkin’s Disease, Aplasticanaemia and primary immune deficiencies are just a few of the lengthy list of diseases in Sri Lanka for which Bone Marrow Transplantation would equal to life saving. However, due to the absence of a National Bone Marrow Donor Registry, the options are limited in the field of BMT.
The NCIM (National Cancer Institute, Maharagama) and NBTS (National Blood Transfusion Service) formulated a 5 year plan under the fostering of St. Vincent’s Hospital Sydney to make Sri Lanka competent in stem cell transplantation. This project was pioneered by the Sri Lankan community in Canberra who enthusiastically worked to make it a reality. A staged introduction of services would be implemented to perform the first autologous stem cell transplant in Colombo in late 2016. Subsequent training of staff for tissue typing and establishment of a Marrow Donor Registry (BMDR) would then lead to an allogeneic stem cell transplantation in 2016-17 with an initial emphasis on sibling transplants.
Today Sri Lanka is in her initial stage in the field of BMT. And since the first public sector BMT that took place in 2016 under the mentorship of St. Vincent’s Hospital Haematology team, the NCIM has performed over 50 autologous stem cell transplants. However, the autologous stem cell transplant is a curative treatment only for certain conditions like myeloma and lymphoma. There exists a plethora of other conditions which demand allogeneic BMTs.
“We need to step up to the next stage where sibling donor transplant, Matched Unrelated Donor (MUD) transplants and haploidentical transplants are the modes of choice.
Not all patients have matched siblings as donors. Full matched unrelated donors (MUD) are preferred to Half matched donors (Haplo-identical) considering overall outcome and management in some centres,” explained Dr. Nilmini Hettiarachchi of NBTS who is presently completing her fellowship in Transfusion/Apheresis and BMT at St. Vincent’s Hospital Sydney.
according to a recent island-wide survey approximately 3000 patients suffer from severe Thalassaemia in Sri Lanka
According to the latest WHO data published in 2017, Leukemia deaths in Sri Lanka reached 781 or 0.62% of total deaths. The age adjusted Death Rate is 3.59 per 100,000 of population, ranking Sri Lanka 106th in the world. Due to the absence of a National Bone Marrow Donor Registry, the options are limited in the field of BMT. Hence, for the majority of local leukaemia patients, chemotherapy and regular blood transfusions are all that could be offered, but these are merely control and supportive care measures and far from remedial.
Every year, 100,000 children are born with Thalassemia across the world. And according to a recent island-wide survey approximately 3000 patients suffer from severe Thalassaemia in Sri Lanka. Moreover, roughly 80 new patients are born each year. The majority of them have beta (β)Thalassaemia major which is a genetic defect that causes dysfunctional red blood cells. The hallmark of treatment is regular blood transfusion with iron chelation therapy for the transfusion-associated iron overload and, supportive care to treat complications of iron overload.
Although most Thalassaemic births occur in the North Western province and North Central province, no part of Sri Lanka can be considered ‘Thalassaemia free’.
The Sri Lanka Journal of Child Health 2018 presents Allogeneic Haematopoietic stem cell transplantation (HSCT) as the only available cure for Thalassaemia. The first HSCT for Thalassaemia was performed in 1982 and over 3000 HSCTs worldwide have been performed since. Best outcomes with overall survival of 90% and disease free survival of over 80%, are reported when transplanting haematopoietic stem cells (HSC) from HLA-matched sibling donors. However only about 10% of Thalassaemia patients are fortunate to have HLA- matched sibling donors, which limits the usefulness of this treatment option.
The journal added that, a decade ago, expenditure on the management of Thalassaemia patients accounted for approximately 5% of the health budget of Sri Lanka. This figure has remained static since. Despite this challenging financial environment, the NCIM and NBTS undertook the NBMDR project.
“We have over 3000 transfusion dependent Thalassaemia patients who depend on blood transfusions every 3- 4 weeks. These patients die of complications related to the frequent transfusion and associated iron overload at the prime of their age. In Sri Lanka only a couple of patients lived to the age of 35. BMT offers them a new life,” Dr.Hettiarachchi stated.
It is true that the Private sector offers BMT treatment through both autologous and allogeneic methods. But at a cost. There are international donor registries that are accredited by the World Marrow Donor Association where donors are registered and their tissue typing is done and uploaded in a data base for use in the event of a HLA (Tissue Type) matching patient demands.
Accessing International marrow registries for lower and middle income countries like Sri Lanka in the public health sector is an impossible task as the cost burden is enormous and not sustainable in the long run.
For the majority of the nation therefore, a National Marrow Donor Registry poses as the bridge between life and death.
“If we do not have our own National Donor Registry, where can we find matching donors for our patients from? Yes you still can find donors, but at a cost you and I cannot even dream of. The international donor registries are ready to find the donors and transport the stem cell products for around USD 25000- 50000 or even more. Mind you, this is only the stem cell product. What about the transplant, chemotherapy, post-transplant care, nutrition, long term follow-ups. This may not be an issue for the upper middle class and the rich people of the country whose medical insurance covers their cost, but this is certainly unthinkable for the majority of people in our country.”Dr. Hettiarachchi shared.
This project was pioneered by the Sri Lankan community in Canberra who enthusiastically worked to make it a reality
The purpose of setting up a bone marrow donor registry in Sri Lanka is to ensure that the best matching marrow donor is available for the required disease. This matching will give the clinicians the assurance of the ability to be able to conduct successful searches and find matching donors so that they may proceed in the transplant field with confidence.
Logistical and technical shortcomings have delayed the establishment of a NBMDR all these years. Starting a donor registry involves more than simply recruiting adult volunteer donors.
Creating robust information technology and finance systems, assessing the feasibility of establishing a registry in the country of choice, evaluating the status of unrelated donor transplantations, need for unrelated donors, and whether there might be existing registries in that country are major factors that need to be considered. The optimum size of the registry, strategies for recruiting donors and identifying how to perform tissue typing methodology need to be well planned. A registry must ensure that search requests, donations and shipments are performed within the legal requirements of the country it’s based at. Donor Identity should be confidential and donor protection guaranteed.
Initial investment in a good database and infrastructure which include an office premises, ongoing funding for staff salaries, donor expenditures etc is crucial. The Australian Bone Marrow Donor Registry (ABMDR) for example consists of twenty one staff members under one director who are involved in IT staff, Search coordinators, Finance officers, Medical officers and Data Entry operators for documentation, quality control and accreditation purposes. However, in Australia where around 360 transplants are done per year, they need to cater to a higher demand. The ABMDR has over 170,000 volunteer donors and 70% of the marrow is still being imported from international registries. With Sri Lankan population count being close to Australia’s we need to adopt a similar, but scaled-down process when setting up our own National Bone Marrow Donor Registry.
Previous proposals have failed on account of a lack of expertise and facilities. However the team at NCIM is now confident that with trained personnel and required facilities they’re inching closer to their goal. Once Sri Lanka sets up her own Bone Marrow Donor Registry, Sri Lankans will gain automatic access to the Bone Marrow Donors Worldwide (BMDW). And becoming a member of the WMDA (World Marrow Donor Association) is a vital part in a National Marrow Donor Programme.
“For a country like Sri Lanka that’s still developing amidst enormous financial strains, we need to move fast to establishing the NBMDR. Sri Lankans are people with great altruism and generosity, ready to donate , with the experience in the National Blood Transfusion Service where we have a very good blood donor population with 100% voluntary blood donations this is an achievable task ” Dr. Hettiarachchi added.
On this account, voluntary donations of blood, blood products, human tissue, organs etc. may be expected from our nation in abundance. Therefore arousing public awareness regarding the country’s present inadequacy and the need for their cooperation is the first step towards establishing a National Bone Marrow Donor Registry in the country.
According to the latest WHO data published in 2017, Leukemia deaths in Sri Lanka reached 781 or 0.62% of total deaths
All these processes need informed consent from the donor/guardian. Strict legislative requirements should be in place for the safety of the donor and the patient with confidentiality maintained.