Reply To:
Name - Reply Comment
Did Sri Lanka ignore the risk?

A deserted Minuwangoda
 COVID-19 is not over yet. At least it was made clear with the discovery of an isolated patient from a garment factory in Minuwangoda, which is being described as the first community case after two months.
COVID-19 is not over yet. At least it was made clear with the discovery of an isolated patient from a garment factory in Minuwangoda, which is being described as the first community case after two months.
But opinions are divided on the medical front with some medics ascertaining that community spread has begun while certain others continuing to claim that Sri Lanka is doing alright. At the time the article was written, around 88 workers at the factory have tested positive for COVID-19 while PCR tests had been conducted on at least 2000 persons including close contacts of the patient and school children. Security measures have been beefed up and curfew has been imposed in Divulapitiya, Minuwangoda and Veyangoda Police divisions.
Sharing their thoughts with the Daily Mirror, some medical experts working on the front lines reiterate on the fact that no community spread has begun. But others warn on strengthening weaker points such as PCR testing.
Not a community spread

The definition of a community spread is identifying cases here and there with no link to one another
Dr. Sudath Samaraweera
However Chief Epidemiologist at the Ministry of Health’s Epidemiology Unit Dr. Sudath Samaraweera confirmed that the new case doesn’t fall into the definition of a community spread. “The definition of a community spread is identifying cases here and there with no link to one another. But this infection happened from a cluster.” said Dr. Samaraweera.
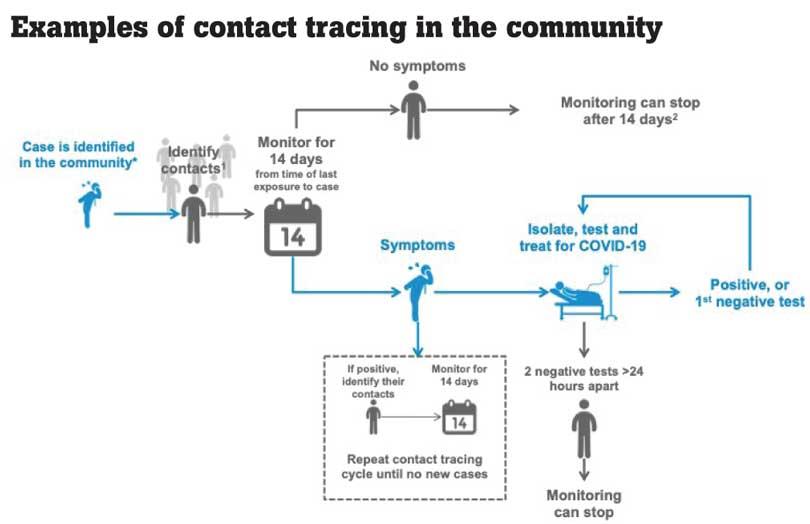
When asked if this is a sign of a second wave, Dr. Samaraweera said that if people don’t adhere to health guidelines, the outbreak of a second wave is highly likely. “Therefore contacts need to be traced and controlled,” he added.
Resources are precious

It’s always advisable to avoid gatherings in small spaces. People with respiratory illnesses shouldn’t go to work
Dr. Jude Jayamaha
“Since it’s a novel virus we still don’t know the source,” opined Dr. Jude Jayamaha, Chief Virologist at the Medical Research Institute. “It’s always advisable to avoid gatherings in small spaces. People with respiratory illnesses shouldn’t even go to work.” affirmed Dr.Jayamaha.
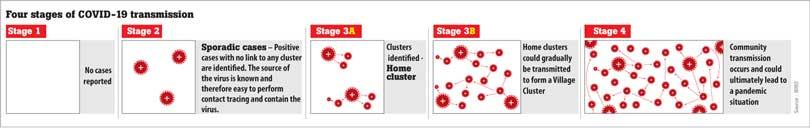
When asked if this is a sign of a community spread he said that technically speaking there is no community spread. “We are not even in Stage 3 A when reviewing the stages explained by the WHO. Therefore people have to continue adhering to health guidelines, maintain physical distancing and help the authorities to control the spread.
He further said that the Coronavirus is not a highly mutable virus like HIV or influenza. “The reproductive value or R0 value for COVID-19 is 5.4. We are continuing PCR testing, but that too is only part of the strategy. Some people who test negative could be positive and vice versa. We also need to have a reserve because our resources are precious. If new clusters are identified there has to be space in the ICUs to admit patients.” said Dr. Jayamaha.
PCR testing - The weakest point

This case was never suspected. So now we have to shift the focus to influenza patients
Dr. Ruvaiz Haniffa
“But this case is coming after a long time and therefore, how can it be linked to any cluster?” questioned Dr. Ruvaiz Haniffa, Consultant Family Physician and Head of the Family Medicine Unit at the Colombo University Medical Faculty. “For the past three weeks I’ve seen many patients with Influenza-Like-Illnesses (ILIs), but we were never looking at these patients before. A patient with an ILI would go to a general practitioner instead of a pulmonologist. But we have to include primary care physicians in order to locate these patients. The Government issues alerts regarding dengue, but why can’t they do it for COVID-19 patients? Testing is sine qua non to trace COVID-19 patients. This case was never suspected. So now we have to shift the focus to influenza patients and patients with other respiratory illnesses. The Government has taken control over testing, but why can’t they include private practitioners too? In countries like Hong Kong, private hospitals are conducting PCR tests under the Government’s supervision. So we have to reintroduce, expand and sustain testing. There are 47 million patients opting for private OPD care and around 30% of them come with a cough or cold. The Government has nationalised the disease.” said Dr. Haniffa, former President of Sri Lanka Medical Association.
He further said that PCR testing has become the weakest point. “The Government has to empower primary care physicians, but they have been excluded from the system. So we have to reinforce solid practices”, he said.
Playing Russian Roulette with public lives?

In a garment factory, most workers are also young, so we should expect a high incidence of infection without symptoms
Dr. Ravindra Rannan- Eliya
“We have to recognise that as long as the COVID-19 pandemic continues, we can never declare victory against COVID-19 in Sri Lanka,” opined Dr. Ravindra Rannan-Eliya, Executive Director, Institute for Health Policy. “To do so is to fool ourselves and the public. An undetected imported case leading to an outbreak is a constant risk, and could always lead to a second wave. The only protection against this risk is to make testing of people with respiratory symptoms or fever the new normal. By not doing so, we are playing Russian Roulette with the lives of the public, our businesses and the education of our kids.” affirmed Dr.Rannan-Eliya.
He further said that however good our airport quarantine procedures, it is always possible for a positive case to get through and later cause a hidden outbreak. “14 days observation during quarantine + 2 PCR tests + 14 days home isolation is not 100% guaranteed to pick up all infected cases. This is not an issue of competence; it simply reflects the biology of the virus. We have known this from the beginning. Some cases will slip through, and this has to be expected.” added Dr.Rannan-Eliya.
“Our quarantine procedures are even now not 100% safe, as indicated by the recent incident involving Russian air crew in Hambantota. Some countries require all air crew to travel under escort to government-managed accommodation and then isolate in those locations till they leave. Air crews are thought to be one source of the second wave in Hong Kong. We were not paying attention.
“Several countries that effectively crushed COVID-19 and have effective quarantine procedures similar to Sri Lanka’s have now suffered outbreaks due to infected cases getting through. These include China, Bhutan, Vietnam, Australia and probably New Zealand. This has to be regarded as inevitable. A question of when and not if.
‘Therefore, in order to keep the country safe, we have to assume that cases will slip through and then cause hidden outbreaks that over the period of weeks could grow to number several hundreds. Because our population is younger than in Europe and since most young adults show no symptoms, an outbreak involving young adults will also spread further before detection. This is what happened in Kandakadu. In a garment factory, most workers are also young, so we should expect a high incidence of infection without symptoms. “We should treat hidden outbreaks as being inevitable, and plan accordingly. The only effective strategy to manage this risk is intensive, continuous testing of people in the community who have respiratory symptoms or fever, as these are the people most likely to have hidden COVID-19 infection. Testing people randomly in the community is a complete waste of time. Hong Kong tests all patients at its OPD with these symptoms, plus others at private GP clinics. Other countries like Australia and New Zealand actively encourage people with coughs and colds, or even a “scratchy throat” to get tested.” said Dr.Rannan-Eliya.
The Health Ministry does some testing like this, but it is on a small scale, not systematic and more importantly not adequate. The evidence is there in the Kandakadu outbreak, and again now in Gampaha. For example, New South Wales in Australia did 150,000 PCR tests in the community during the past two weeks for its 8 million people. This compares with just 25,000 in Sri Lanka for 22 million people. We need to increase our routine testing by tenfold. Yes, it will cost money, but we will save far more by not having to impose lockdowns, curfews, close factories and schools as we now end up doing.
In conclusion he added that if MOH puts in a testing and isolation programme akin to Asian countries like China, Vietnam and Hong Kong, or like Western nations such as Australia and New Zealand, Sri Lanka doesn’t have to demand too much from the public other than coming for testing when they have symptoms. “We could probably manage most of the time without lockdowns, school closures or even masks. However, since we don’t have such a programme, the public should take precautions, such as wearing masks, maintaining social distancing, etc, and going to the hospital asking for a test if they have any respiratory symptoms or fever that cannot be explained.” said Dr.Rannan-Eliya
A normal phenomenon in the Dance phase

She may have travelled in three-wheelers and used public transport
Dr. Haritha Aluthge
Expressing his views about the new situation, Dr. Haritha Aluthge, Secretary of Government Medical Officers’ Association said it is normal to see isolated cases in the Dance phase. “We explained about the Hammer and Dance theory since the outbreak of COVID-19. There have been 1700 workers in this garment factory and around 683 workers who worked in the same floor as the patient are at risk. So there’s a possibility for more people to test positive within the next 72 hours.” warned Dr. Aluthge.
“The patient is from Galle and her daughter was also infected with the virus, so people around the country are exposed to a risk,” he added. “This means that she may have travelled in three-wheelers and used public transport. Therefore more contact tracing should take place during this period. Apart from that more aggressive testing should take place and they should be repeated in three days, one week or 10 days. After 72 hours we can assess the risk and formulate responses accordingly.” said Dr. Aluthge.
 He further said that the public too has a huge responsibility in helping authorities contain the spread. “Just because school holidays were declared the public should not go on unnecessary trips. They should look after the elderly population and especially patients with non-communicable diseases (NCDs). There have been over 100,000,000 deaths due to COVID and around 96.2% of cases were co-related with an NCD. Therefore COVID-19 is what is visible to the naked eye, but the underlying risk factor could be a NCD.” he added.
He further said that the public too has a huge responsibility in helping authorities contain the spread. “Just because school holidays were declared the public should not go on unnecessary trips. They should look after the elderly population and especially patients with non-communicable diseases (NCDs). There have been over 100,000,000 deaths due to COVID and around 96.2% of cases were co-related with an NCD. Therefore COVID-19 is what is visible to the naked eye, but the underlying risk factor could be a NCD.” he added.
According to Dr. Aluthge students at the Wickramarachchi Ayurveda Institute and Kelaniya University were sent home, but ideally they should have been kept in self isolation. “Before taking such decisions its better if authorities could consult local public health inspectors, medical officers of health and other medical officials.” he said.
When asked if there was a capacity to include patients in ICU care if there’s a sudden increase, Dr. Aluthge said that there were only 120 such patients. “But all those hospitals that were dedicated to taking care of COVID-19 patients got normalised.
So these facilities should again look at paying more attention to offering specialised care for COVID-19 patients. What’s worrying is the capacity at quarantine centres because they have reached a near maximum capacity. If more clusters are found we may have to find new places to put up quarantine facilities.” he said.