Reply To:
Name - Reply Comment
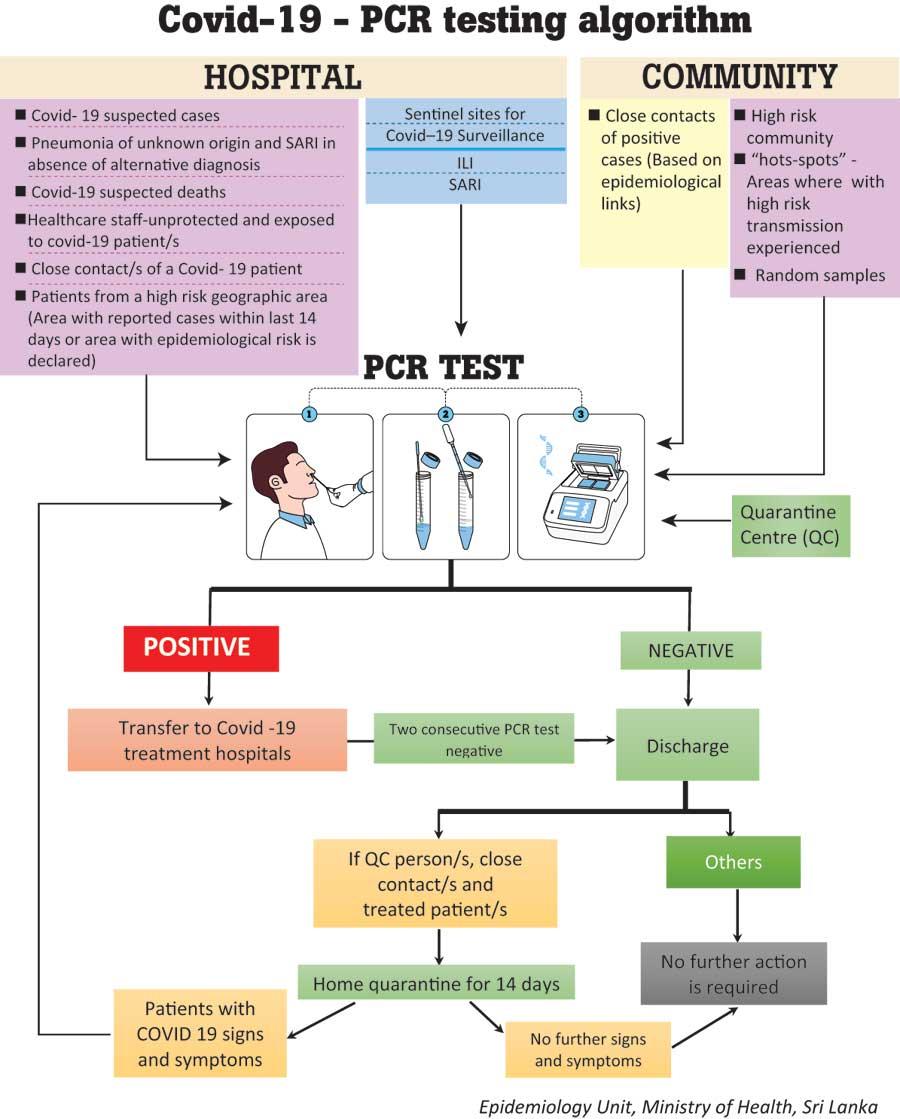
Nearly 400,000 PCR tests have been carried out to detect positive cases of the Minuwangoda cluster. As means of expanding the testing capacity, select hospitals in the private sector have also been allowed to conduct tests at varying rates. It has however been observed that results have varied in certain instances.

Almost all laboratories go through a quality control process
Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) is carried out with samples such as swabs obtained from oropharynx and nasopharynx or sputum. This test detects genetic materials of the virus (RNA). According to  research studies, results are for the identification of SARS-CoV-2 RNA. The SARS-CoV-2 RNA is generally detectable in respiratory specimens during the acute phase of infection. Positive results are indicative of the presence of SARS-CoV-2 RNA; clinical correlation with patient history and other diagnostic information is necessary to determine patient infection status. Positive results do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of disease.
research studies, results are for the identification of SARS-CoV-2 RNA. The SARS-CoV-2 RNA is generally detectable in respiratory specimens during the acute phase of infection. Positive results are indicative of the presence of SARS-CoV-2 RNA; clinical correlation with patient history and other diagnostic information is necessary to determine patient infection status. Positive results do not rule out bacterial infection or co-infection with other viruses. The agent detected may not be the definite cause of disease.
Negative results do not preclude SARS-CoV-2 infection and should not be used as the sole basis for patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information.
Ministry of Health secretary Dr. Jayaruwan Bandara explained where people can get PCR tests done and why 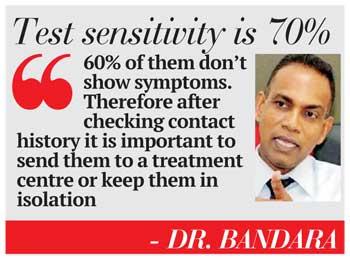 there could be varied results.
there could be varied results.
Q Where can people do PCR testing?
There are around 20 Government hospitals designated to conduct PCR tests while there are selected private hospitals that also conduct these tests. It is the Public Health Inspectors (PHIs) who send samples to Government hospitals.
Q Can a person do a PCR test on his/her own?
Yes at a private hospital.
Q Sometimes people test positive and then results become negative in the second test. Could you explain why?
This is because test sensitivity is only 70% and it applies to tests being done around the world. Therefore contact history is important at this point. During screening there could be one result and during a random testing there could be another result.
Q What could be done about people who don’t show signs, but test positive for COVID?
60% of them don’t show symptoms. Therefore after checking contact history it is important to send them to a treatment centre or keep them in isolation.
"Negative results don’t preclude SARS-CoV-2 infection and should not be used as the sole basis for patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information"
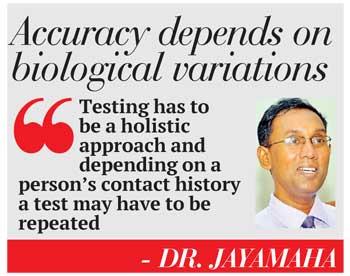 According to Dr. Jude Jayamaha, Consultant Virologist at the Medical Research Institute, theoretically it could be 100% specific, but when you shift to a lab or the field, the results depend.
According to Dr. Jude Jayamaha, Consultant Virologist at the Medical Research Institute, theoretically it could be 100% specific, but when you shift to a lab or the field, the results depend.
There are three factors to consider :
“There’ll be a difference in samples collected from a community and that of a patient in a closed setting. If the first sample is negative and the clinical suspicion is high you need to repeat the test. Almost all laboratories go through a quality control process. Therefore the sample, batch and machine are quality controlled. Laboratory variations are regularised by a standard method.” he added.
He further said that COVID-19 secretion varies. “There could be high secretions as well as low secretions. Those having low secretions would test positive the first time and negative the second time. Testing has to be a holistic approach and depending on a person’s contact history a test may have to be repeated. Therefore depending on biological variations of the virus, the results will vary.” he said.