Reply To:
Name - Reply Comment
The article is based on an interview by Jayam Rutnam of the San Gabriel Valley Examiner with Dr. Deepthi Jayasekara of Glendora, California. Dr. Jayasekara is a specialist in Infectious Diseases, Foothill Infectious Diseases, Claremont, Ca., Chair, Infection Control, Emanate and San Dimas Hospitals, Clinical Professor, Western and Touro University.
Every year, there are millions of cases of regular coronavirus infections reported, causing common cold/upper respiratory infections. 30% of common colds are caused by coronaviruses. Historically, pandemics are caused by influenza and coronavirises. Examples are 1918 Spanish flu, Asian Flu in 1950’s, Hong Kong flu in 1960’s and H1 N1 swine flu in 2009, all caused by Influenza viruses. SARS, MERS and 2019 Novel Coronavirus were caused by Corona viruses.

Dr. Deepthi Jayasekara
Current Coronavirus epidemic shows signs of high infectivity (indicating how contagious the virus is) but low mortality (case fatality) is around 4%. SARS mortality was 10% and MERS 35%.
The current outbreak has caused over 700 deaths (constantly evolving), 99% in China. Over 35,000 people have been sicked by the virus thus far. The first American died yesterday and one Filipino and another person from Hong Kong succumbed to the infection. The rest of the deaths occurred in China so far. Unfortunately,the whistle blower doctor, a 35 year old ophthalmologist from China also passed away last week.There have been cases reported all over the world including 27 countries.
We, as Infectious Disease specialists, have reiterated that the virus is contagious, but the fear can be even more contagious. Panic can make the situation much worse. All the doctors’ 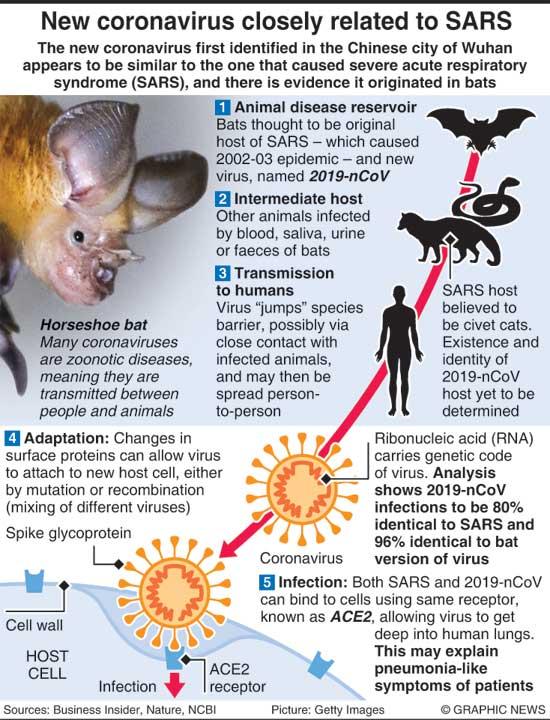 offices and hospitals have been prepared for potential patient with a protocol and a check list to follow as closely monitored by Health Department and CDC. Given the low mortality reported so far, we do not need to panic unnecessarily at this time. Most experts do not recommend wearing masks in public here for reasons that are known to all of us. Furthermore, ID specialists also reiterate that Influenza kills 30,000-40,000 every year and they advocate every person over six months to be vaccinated against influenza every year. We constantly emphasize the importance of hand hygiene and respiratory hygiene to prevent all respiratory infections.
offices and hospitals have been prepared for potential patient with a protocol and a check list to follow as closely monitored by Health Department and CDC. Given the low mortality reported so far, we do not need to panic unnecessarily at this time. Most experts do not recommend wearing masks in public here for reasons that are known to all of us. Furthermore, ID specialists also reiterate that Influenza kills 30,000-40,000 every year and they advocate every person over six months to be vaccinated against influenza every year. We constantly emphasize the importance of hand hygiene and respiratory hygiene to prevent all respiratory infections.
"Today both the Journal of the American Medical Association (JAMA) and the Centres for Disease Control and Prevention’s (CDC’s) Morbidity and Mortality Weekly Report (MMWR) published initial clinical guidelines, which aim to help US healthcare providers identify and correctly handle suspected cases involving the novel coronavirus (2019-nCoV)"
Today both the Journal of the American Medical Association (JAMA) and the Centres for Disease Control and Prevention’s (CDC’s) Morbidity and Mortality Weekly Report (MMWR) published initial clinical guidelines, which aim to help US healthcare providers identify and correctly handle suspected cases involving the novel coronavirus (2019-nCoV).
2019-nCoV was first identified in Wuhan, China, the country that continues to report more than 99% of cases. US officials today confirmed the 12th US case. The virus, which shares similarities with both MERS-CoV (Middle East respiratory syndrome coronavirus) and the SARS (severe acute respiratory syndrome) virus, causes acute respiratory distress syndrome in about one third of patients that requires intensive care, write Carlos del Rio, MD, of the Emory University School of Medicine, and Preeti N. Malani, MD, MSJ, of the University of Michigan, in the JAMA article. Most clinical presentations of the virus will be nonspecific and include fever and a dry cough, with about 30% of patients also experiencing shortness of breath. Based on case reports from China, the median age of patients is between 49 and 56 years, and cases in children have been rare.
“When a patient presents with fever and respiratory symptoms (in particular a dry cough), clinicians should obtain a detailed travel history. If the patient has a history of travel to Hubei Province in the last 14 days, they should be considered a Person Under Investigation (PUI),” the authors write. As should patients who had any travel to China in the preceding 14 days, and any patients who had close contact with a confirmed 2019-nCoV patient.
Upon identifying a PUI, clinicians should immediately notify their health facilities’ infection prevention team and state health authorities. If the novel coronavirus is suspected, the patient should have a face mask placed immediately, and healthcare practitioners should wear N95 respirators.
“What interventions will ultimately control this outbreak is unclear because there is currently no vaccine, and the efficacy of antivirals is unproven. However, basic public health measures such as staying home when ill, hand-washing, and respiratory etiquette including covering the mouth and nose during sneezing and coughing were effective in controlling SARS,” which also originated in China, the authors conclude. CDC suggests special isolation, if possible in MMWR, CDC experts’ interim clinical guidelines are based on the management and prevention of respiratory illnesses, including influenza, MERS, and SARS.
The MMWR guidelines identify the same three types of PUIs—symptomatic patients with (1) a travel history to Wuhan, (2) a travel history to China, or (3) close contact with a confirmed 2019-nCoV case—but also suggest patients be immediately placed in some form of medical isolation.
The writer could be contacted on [email protected]