10 Oct 2016 - {{hitsCtrl.values.hits}}
Today marks the World Mental Health Day under the theme ‘Dignity in mental health-Psychological and mental health first aid for all’. The aim of this year’s theme is to prepare people to confidently tackle the stigma, isolation and discrimination that continue to affect those who suffer from mental health conditions, their families
and caregivers.
 Psychological first aid covers both psychological and social support. Therefore, investment in psychological first aid is an important component of the longer-term effort to ensure that anyone in acute distress due to a crisis is able to receive basic support and for those who require more than psychological first aid, will receive additional support from health, mental health and social services.
Psychological first aid covers both psychological and social support. Therefore, investment in psychological first aid is an important component of the longer-term effort to ensure that anyone in acute distress due to a crisis is able to receive basic support and for those who require more than psychological first aid, will receive additional support from health, mental health and social services.
Mental, neurological and substance use disorders are common across all communities and age groups and countries, irrespective of income levels. Depression for example affects 350 million persons globally and is the single largest contributor to years lived with disability. The cost of depression was estimated to be at least US $ 800 billion in 2010 in lost economic output and is estimated to more than double by 2030. According to the Mental Health Atlas 2014, only a mere 68 percent of the World Health Organisation (WHO) member states have a stand-alone policy or plan for mental health. With 14 percent of the global disease burden attributed to these mental disorders, 75 percent of those people in many low-income countries do not have access to the treatment they require. Implementation of policies protecting people with mental disorders is weak and family members are partially involved in caring for them.
This article outlines the mental health status in Sri Lanka and highlights the issues faced by both patients and caregivers. It further reiterates the urgency for a comprehensive and integrated response to mental health and care services.
Status in Sri Lanka
Sri Lanka, unlike other WHO member states, initiated a mental health legislation in 1873, which was later revised in 1956 with legal provisions concerning mental health welfare, disability and general health legislation. An official mental health policy was approved and published in 2005 and further revisions to the policy are still underway.
A significant number of people in the country suffer from psychiatric illnesses and serious mental disorders. Available data suggest that about 10 percent of the population are afflicted with more common psychiatric ailments.
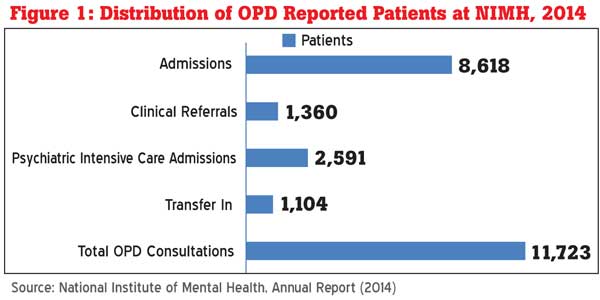
Figure 1 depicts a total of 11,723 OPD patients were reported in 2014 by National Institute of Mental Health (NIMH), of which 83 percent were admitted. Amongst the admissions, 2,591 patients (26 percent) urgently required psychiatric and intensive care and 1,341 patients (13.6 percent) were transferred to the institute from other hospitals. Given that treatment is centralized and only available in the cities and most patients are reluctant to obtain medication, they enter hospital at the late stages of their illness, which implies that they require intensive care.
From a total of 7,062 patients (Figure 2) admitted in 2014, 62 percent of patients admitted were within the age group of 17-49 years, of which 2,970 patients were male. The country also has one of the highest suicide rates amongst youth with recent protracted conflict and the tsunami aggravating mental health needs. The suicide rate for males is 44.6 per 100,000 population, while for females it’s 16.8 per 100,000 population. Suicidal rates have increased in the last two decades with approximately 10 suicides reported islandwide daily, with half the victims having suffered from depression.
The high incidence of suicide stems from impulsiveness and the inability to cope, which has resulted in the major causes of death among youth.
Hurdles in mental healthcare
Stigma, isolation, discrimination
Stigma is an overarching barrier associated with mental disorders worldwide but more prominent in Asian countries where communities are family-orientated. Many Asian families including Sri Lankan families hide mental illness from society to avoid discrimination in terms of marriage engagements and employment prospects. Even when help has been sought, evidence show that reintegration into families is poor, due to the associated stigma. This leads to a vicious cycle whereby people with mental illnesses continue to be undiagnosed, leading to isolation, particularly if action is not taken to understand and support families experiencing mental health
care problems.
Conflicts in service provision
The absence of knowledge among patients, families and friends underlies the stigma associated with the disease and also acts as a barrier to seek mental health services. Patients often seek traditional medicine first prior to attending community-based mental health services thereby delaying early diagnosis and treatment. Given that community-based mental health services are not readily available throughout the country, traditional medicine is the primary choice. However, patients often prefer if both traditional healers and western methods of treatment such as community mental health caregivers co-exist and
work together.
Poor funding and scarcity of human resources
Mental healthcare in Sri Lanka is plagued by poor funding and a scarcity of trained human resources. Services provided are centralized and only available in cities. With only 67 consultant psychiatrists in the country and approximately 200 patients visiting the Colombo National Hospital on a daily basis, the inequality in the provision of care is a serious cause for concern. The deficit of trained mental health workers is worsened by geographical inequity, with the majority of psychiatrists located in the Western Province. A large proportion of postgraduates trained in psychiatry in the last few decades, have not returned to Sri Lanka upon their completion of their overseas training. Others have worked in Sri Lanka for a few years and migrated overseas for better prospects. Also, the absence of a proper referral system and poorly developed multidisciplinary teams make it difficult for psychiatrists to deliver
services optimally.
Although community-based mental hospitals are considered to be more accessible and reduces the reliance of tertiary care, their services seems to be provided in an ad hoc manner. At the same time, outpatient clinics in tertiary care hospitals have inherent problems. Lack of a culturally appropriate service to accommodate the needs of diverse patients, fear of experiencing discrimination in the treatment setting, language and communication barriers, lack of familiarity with mainstream mental health services are many of the hurdles faced by mental health patients and their families.
Way forward
Addressing the diverse and complex mental health issues requires multiple approaches to intervention and support provision. This demands the development of professional services such as psychiatrists and community-based mental health services to supplement the traditional societal coping strategies, dealing with interpersonal and social problems such as stigma and discrimination, which cause considerable suffering to individuals and their families. Therefore, the Government of Sri Lanka should consider providing a comprehensive and integrated response to mental health and care services, which educate people on mental health issues in community-based settings and implement strategies to create awareness on preventing mental
health issues.
(Yolanthika Ellepola is a Research Assistant at the Institute of Policy Studies of Sri Lanka)
10 Jan 2025 44 minute ago
10 Jan 2025 49 minute ago
10 Jan 2025 2 hours ago
10 Jan 2025 2 hours ago
10 Jan 2025 2 hours ago