03 Sep 2021 - {{hitsCtrl.values.hits}}

 Like many other countries, Sri Lanka faces numerous challenges in the battle against COVID-19. The pandemic has caused deep uncertainty and presented a colossal challenge for the country’s healthcare system.
Like many other countries, Sri Lanka faces numerous challenges in the battle against COVID-19. The pandemic has caused deep uncertainty and presented a colossal challenge for the country’s healthcare system.
With the rapid increase in cases and the emergence of new variants, Sri Lanka began to face shortages of medical resources, including hospital beds and medical equipment. The vaccination programme was beset with a host of problems early on, due to the irregular and inconsistent supply of vaccines, disorganised deployment and deviation from the scientifically agreed prioritisation.
There was also alleged misreporting of COVID-19 daily statistics in the Gampaha district and Eastern province. The absence of real-time data acted as a hindrance to obtain a reliable risk assessment in the country.
Against this backdrop, this article examines the gaps in the ongoing pandemic control programme and outlines ways to bridge these gaps so that more lives could be saved from COVID-19.
COVID-19 vaccination programme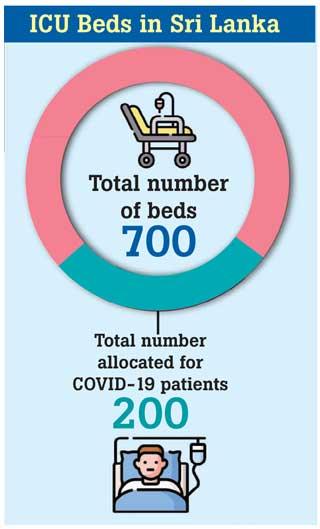
By mid-August 2021, more than 12 million Sri Lankans (55 percent of the population) had been vaccinated with at least the first dose. Other than the delayed supply of vaccines, there were issues related to getting approval for vaccine use and the vaccination prioritisation process.
Moreover, many people were seen queuing up at vaccination centres aggravating health risks, due to the lack of a properly planned system for vaccine deployment and the lack of an online appointment system.
More recently, the government has taken several measures to improve the rollout, including expediting the procurement process and improving administration with the support of the defence services.
Gaps in pandemic control
Sri Lanka’s rate of COVID-19 screening has remained inadequate to prevent the spread of the virus. Systematic surveillance is crucial for the rapid identification and detection of suspected COVID-19 cases. With newer variants found to be more transmissible and deadlier, there is a need to identify mutants and track the nature of transmission. Currently, the University of Sri Jayewardenepura is the only institution equipped with laboratory facilities to conduct genomic sequencing to identify new variants.
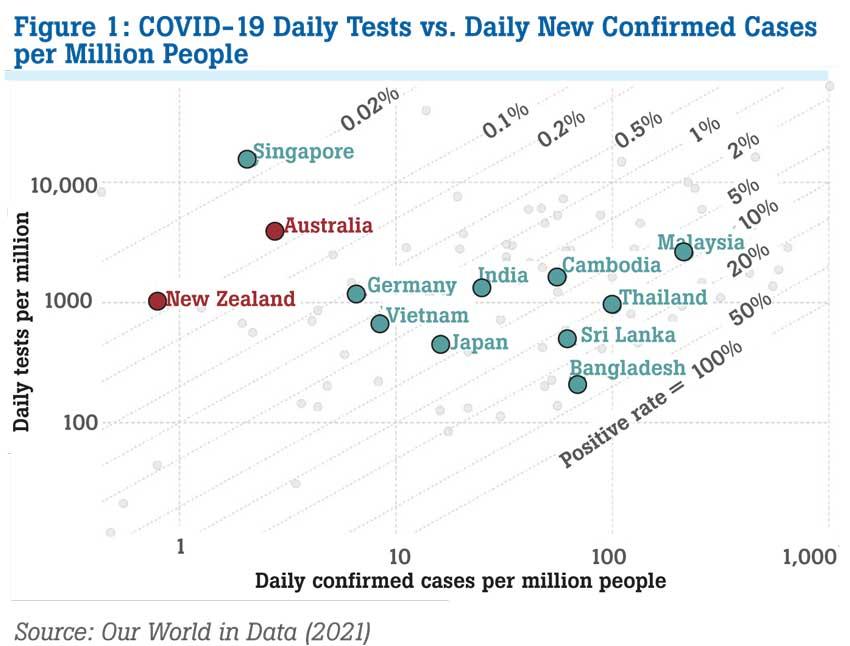
Countries like Singapore, New Zealand and Australia systematically monitor the pandemic through extensive testing and contact tracing. As shown in Figure 1, these countries are conducting 10-100 times more tests than other countries, with a similar number of new confirmed cases. Sri Lanka’s extent of testing relative to the scale of the outbreak (positive rate was around 10 percent), is on par with Thailand and Malaysia but lower than India, Vietnam and Cambodia, where the positive rate is below 5 percent.
Further, a major challenge to the existing healthcare system is inadequate ICU beds, ventilators, oxygen supplies and other necessities required to care for patients with severe respiratory failure. The availability of ICU capacity plays a crucial role in critical cases and constant and uninterrupted availability of oxygen supplied beds is needed to avert a disaster.
Currently, less than 200 ICU beds are in isolation units for patients with severe COVID-19 symptoms, whereas just around 700 ICU beds are available in the hospital system of the entire country.
Equally, it is vital to have timely access to real-time data so that meaningful insights can be drawn but due to capacity constraints and administrative issues, PCR test results are reported to be delayed. In some districts, the delays are said to be longer than one week. Thus, delays in generating test results are a grave concern and represent a major obstacle in the COVID-19 control process.
There is a growing need for immediate and accessible healthcare and digital healthcare resources to effectively respond to the challenges posed by COVID-19. However, Sri Lanka’s health information systems are weak and under-funded and the lack of an adequate central health database and IT infrastructure has hampered digital health services.
Towards a stronger healthcare response
The healthcare system has to be streamlined to ensure a successful vaccination deployment and a smooth inoculation programme with online appointments, including over the phone appointment facilities. Parallel to an efficient vaccination programme, an enhanced screening capacity is needed for the rapid identification of COVID-19 cases.
Sri Lanka’s overall COVID-19 screening capacity remains low; therefore, expanding testing and increasing the health sector’s capacity to identify new mutants is vital to curb the pandemic. Random PCR testing too must be carried out in densely populated areas, which are prone to be contagious, thereby taking additional
precautionary measures.
There is a growing concern about the availability of medical supplies in emergency contexts. Sri Lanka has to effectively leverage its limited resources in response to the pandemic. The crisis response has seen local innovation in the manufacturing of ICU beds and lab consumables and there is further scope to encourage local enterprise and innovation for this purpose.
For instance, a team of Sri Lankan scientists recently invented a new PCR test kit using NANO technology, which is said to drastically reduce the testing time from two hours to half an hour. There is now an opportunity to encourage local innovation and local production through such efforts, where they contribute to efficiency gains.
Furthermore, a robust laboratory strategy, which includes laboratory networking, communicating real-time information on COVID-19, quality assurance and adequate workforce capacity is important for rapid detection and case management.
South Korea, for example, practised the disclosure of real-time information on COVID-19 by the government via dedicated websites, mass media, phone messages and mobile apps. Digitalisation of healthcare and effective use of technology for sharing real-time data, contact tracing and surveillance and coordinating the efficient use of clinical resources are vital for successful pandemic control.
It is also necessary to improve systems to manage real-time data and decision-support systems. Improved functional integration and coordination in treatment centres and laboratory services bring in many benefits.
(Priyanka Jayawardena is a Research Economist at the Institute of Policy Studies. Her research interests include education and skills development, labour economics, inequality analysis, health economics and child nutrition. She holds a BSc (Hon) in Statistics and an MA in Economics from the University of Colombo. She can be reached at [email protected])
23 Dec 2024 2 hours ago
23 Dec 2024 3 hours ago
23 Dec 2024 6 hours ago
23 Dec 2024 8 hours ago