This can cause discomfort and changes in your bathroom habits, like cramping, bloating, and diarrhea or constipation. It’s important to know that IBS isn’t a dangerous disease and doesn’t damage your intestines, but it can be quite uncomfortable.
The first step is figuring out which foods seem to worsen your IBS symptoms. This can involve keeping a food diary to track what you eat and how you feel afterwards
By Kshalini Nonis

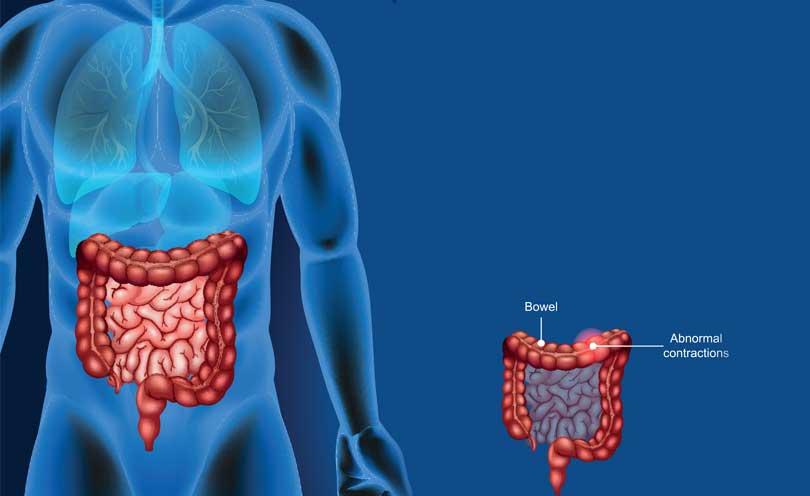
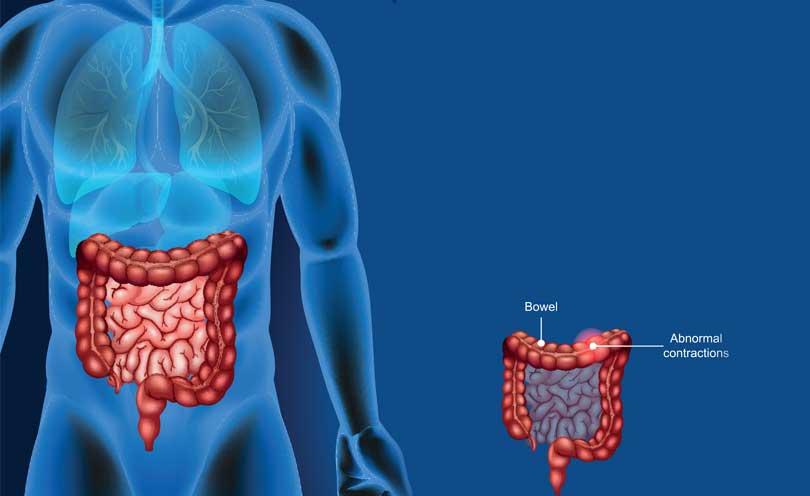
Irritable Bowel Syndrome (IBS), is a group of symptoms that occurs together, including repeated pain in your abdomen and changes in your bowel movements , which maybe diarrhea, constipation, or both.
We had a chat with Dr Uditha Dassanayake, Consultant Gastroenterologist and Hepatologist on IBS.
Q: What is a definition of Irritable Bowel Syndrome (IBS)?
Irritable bowel syndrome, or IBS, is a condition where your intestines are more sensitive than usual. This can cause discomfort and changes in your bathroom habits, like cramping, bloating, and diarrhea or constipation. It’s important to know that IBS isn’t a dangerous disease and doesn’t damage your intestines, but it can be quite uncomfortable.
Q: What causes IBS?
The exact cause of IBS remains under investigation, but researchers believe it’s a complex interplay between several factors affecting how your gut functions. Some of the most important contributors are:
Gut Sensitivity: Your intestines might be hypersensitive to various stimuli. This could include:
Stress: When stressed, your body releases hormones that can affect gut motility (movement of food) and lead to discomfort.
Food Intolerances: While not a true allergy, certain foods might trigger IBS symptoms in some people. Common culprits include dairy products, gluten, or high-fiber foods.
Changes in Routine: Disruptions in your normal sleep patterns, meals, or travel can upset the delicate balance in your gut.
Muscle Imbalances: The muscular contractions in your gut wall propel food along the digestive tract. In IBS, these muscles might be:
Overactive: Leading to cramping, diarrhea, and a sense of urgency.
Underactive: Causing constipation, bloating, and incomplete bowel movements.
Nervous System Miscommunication: The complex network of nerves lining your gut and connecting it to your brain might be sending mixed signals. This can lead to:
Increased Perception of Pain: Even normal gut activity might feel uncomfortable or painful.
Altered Bowel Motility: Inappropriate nerve signals can disrupt the coordinated muscle contractions needed for proper digestion.
It’s important to remember that IBS isn’t caused by a single factor, and it can vary from person to person.
Q: How do you know if you have IBS?
Irritable bowel syndrome (IBS) can be frustrating because there is no single test to diagnose it definitively. Doctors rely on your symptoms and medical history to understand what’s going on.
IBS Symptoms to watch for:
Abdominal Pain and Cramping: This is often the most noticeable symptom, and it can range from dull aches to sharp pains. Interestingly, passing a bowel movement often brings relief.
Bloating: Feeling constantly puffed up or swollen in your abdomen is a common complaint with IBS. It can be quite uncomfortable and lead to tightness in your clothes.
Bowel Habit Changes: This is a hallmark of IBS. You might experience:
Diarrhea: Frequent loose stools that can come on suddenly and urgently.
Constipation: Difficulty passing stools, or stools that are hard and lumpy.
Alternating between diarrhea and constipation: This is also quite common with IBS.
While these are the main symptoms, IBS can also cause:
Feeling Like You Haven’t Completely Emptied Your Bowels: Even after using the restroom, you might have a persistent feeling of fullness or blockage.
Urgency to Have a Bowel Movement: This can be quite stressful, leading to a sudden need to find a bathroom.
It’s important to remember:
There are other more sinister causes like colon cancer or polyps which can cause similar symptoms.
The severity varies from person to person. Some people might have mild, occasional IBS episodes, while others experience more frequent and intense symptoms.
Q: What tests if any should be done?
The diagnosis of IBS hinges on symptoms. There is no single test, but investigations are crucial to rule out other conditions that may mimic IBS.
Stool tests: Exclude infectious causes of diarrhea with tests like ova and parasites (O&P) or stool culture, depending on the suspected culprit.
Blood tests: Can be used to rule out anemia with a complete blood count (CBC) or to check for evidence of infection or inflammation.
Imaging tests (selective): X-rays, ultrasounds, or colonoscopy may be used to exclude colon cancer, inflammatory bowel disease (IBD) or structural abnormalities, especially in patients over 50 or with concerning symptoms (e.g. rectal bleeding).
These tests don’t diagnose IBS directly, but ensure a more serious condition isn’t the underlying cause. Confirming IBS and excluding other possibilities allows doctors to tailor treatment plans and optimize patient outcomes.
Q: What is the treatment for it and can it be cured permanently?
The target of treating IBS isn’t achieving a permanent cure, as it is associated with multiple symptoms, and eliminating all of them completely can be very difficult.
However, there are several effective treatment options that can significantly manage symptoms and improve your quality of life.
The main treatment approaches include:
Dietary Changes: Identifying and avoiding food triggers (like dairy or high-fiber foods) can be very helpful.
Lifestyle Modifications: Stress management techniques like yoga or meditation can make a big difference. Regular exercise is also beneficial.
Medication: Medications like antispasmodics (for cramps), laxatives (for constipation), or antidiarrheal agents (for diarrhea) can provide relief.
Psychological Therapy: In some cases, therapy can address the connection between stress and IBS symptoms.
By working with professionals and exploring these treatment options, you can develop a personalised plan to effectively manage your IBS and feel better.
Q: What type of food should be avoided?
Dietary changes are a cornerstone of managing IBS symptoms.
Identify Food Triggers: The first step is figuring out which foods seem to worsen your IBS symptoms. This can involve keeping a food diary to track what you eat and how you feel afterwards. Common culprits include:
FODMAPs: This group of fermentable carbohydrates (sugars) can trigger bloating and gas in some people with IBS. A low-FODMAP diet can be helpful in identifying specific problematic foods within this group.
Dairy: Lactose intolerance can mimic IBS symptoms. Trying lactose-free options might provide relief.
Gluten: While less common, some people with IBS find gluten-containing grains (wheat, barley, rye) worsen their symptoms.
* Avoid Triggers, Embrace Safe Options: Once you identify your triggers, limit or avoid them. You may have to explore lactose-free dairy products, gluten-free options if needed, and low-FODMAP alternatives for your favorite foods.
Regular, Smaller Meals: Eating smaller meals more frequently throughout the day can be easier on your digestive system compared to a few large meals.
Stay Hydrated: Drinking plenty of fluids throughout the day helps keep your digestive system moving smoothly and can prevent constipation.
Fibre with Caution: While fibre is generally good for digestion, some types of fibre can worsen IBS symptoms for some people. Talk to your doctor or a dietitian about incorporating the right types and amounts of fibre into your diet.
Q: What lifestyle changes should be made?
There are several lifestyle changes that can help in dealing with the symptoms of IBS. These include:
Stress Management: Stress is a major trigger for IBS symptoms in many people. Techniques like yoga, meditation, deep breathing exercises, or even spending time in nature can significantly reduce stress and improve IBS symptoms.
Regular Exercise: Aim for moderate-intensity exercise most days of the week.Exercise helps manage stress, promotes regular bowel movements, and improves overall gut health, all beneficial for IBS.
Sleep Hygiene: Getting enough quality sleep is crucial for overall health and can also positively impact IBS symptoms. Establish a regular sleep schedule, create a relaxing bedtime routine, and ensure a comfortable sleep environment.
Limited Alcohol and Caffeine: Some people find that limiting alcohol and caffeine intake can improve their IBS symptoms.
Q: Is it necessary to see a therapist?
Seeing a therapist for IBS isn’t necessarily mandatory for everyone with the condition. If your IBS symptoms are well-controlled with dietary changes, lifestyle modifications, and medication, therapy might not be essential. However, if you feel stress is a major factor in your IBS, or if IBS is impacting your mental health, then therapy can be a valuable addition to your treatment plan.
There are situations where therapy can be a powerful tool for managing IBS:
Stressful IBS Triggers: If stress significantly worsens your IBS symptoms, a therapist can teach you effective stress management techniques like cognitive behavioral therapy (CBT) or relaxation techniques.
Pain Management: Therapy can teach coping mechanisms for dealing with IBS- related pain and discomfort, improving your overall quality of life.
IBS and Emotional Distress: IBS can sometimes lead to anxiety or depression.
Therapy can address these co-occurring conditions, improving your emotional well-being and potentially reducing IBS symptoms.
Ultimately, the decision to see a therapist is personal. Discussing your concerns with your doctor can help you determine if therapy could be beneficial for you.
Q: Is it correct that IBS can lead to cancer?
IBS does not lead to cancer. However, some of the symptoms of IBS can overlap with those of colon cancer. It is extremely important to rule out colon cancer if any suspicious symptoms are present. (e.g. rectal bleeding, weight loss)
Q: Finally can you give a checklist/summary?
IBS in a nutshell
Irritable bowel syndrome (IBS): Sensitive intestines leading to cramps, bloating, and bowel issues (diarrhea, constipation).
Not dangerous, but uncomfortable.
Cause unknown, likely a mix of factors (stress, food sensitivities, gut issues).
Diagnosed by symptoms and tests to rule out other conditions.
Manageable, not curable: food changes, stress management, medication, therapy (in some cases).
No IBS cancer link, but some symptoms overlap (get checked for rectal bleeding) weight loss, bowel habit changes).
 Irritable Bowel Syndrome (IBS), is a group of symptoms that occurs together, including repeated pain in your abdomen and changes in your bowel movements , which maybe diarrhea, constipation, or both.
Irritable Bowel Syndrome (IBS), is a group of symptoms that occurs together, including repeated pain in your abdomen and changes in your bowel movements , which maybe diarrhea, constipation, or both.