14 Jun 2017 - {{hitsCtrl.values.hits}}

 Though micro-organisms have their uses, invading and infecting our bodies are certainly not one of them! There was a time in the not-so recent past when tuberculosis equalled a preassigned death certificate and leprosy meant that you had to spend your life in an asylum, isolated from civilization.
Though micro-organisms have their uses, invading and infecting our bodies are certainly not one of them! There was a time in the not-so recent past when tuberculosis equalled a preassigned death certificate and leprosy meant that you had to spend your life in an asylum, isolated from civilization.
Then in 1928, Alexander Fleming discovered penicillin in a petri-dish of mould. Penicillin, the first antibiotic was followed up with many other such antibiotics of different classes.Today, with the correct antibiotic taken at the correct time, almost any infection from tuberculosis to pneumonia to meningitis can be cured. However, antibiotic resistance is an ominous threat hanging over the bright skies of medicine, threatening to take us back to the time when infections were not curable through a drug.
Antibiotics are substances capable of weakening or destroying micro-organisms, specifically bacteria and fungi.These differ from the other drug groups because they deal with living organisms, focusing on a feature specific to a certain group of microbes. For example, penicillin focuses on the bacterial cell wall, preventing new cell wall formation, thus making the bacteria vulnerable to the external environment. Antibiotics are different to each other in function and strengths. Some antibiotics do not work on certain bacteria, while some cure infections more effectively than others.
In a perfect world, the same antibiotic, say amoxycillin, will always work for a strep throat, killing all bacteria the same way fever always responds to paracetamol. Fortunately for the bacteria, evolution has come to their help. When an antibiotic is administered, due to the fast reproductive rates of the bacteria, mutations occur to produce organisms that can survive the effects of the antibiotic. In addition to this, in a colony of microbes, there are some organisms with features that can combat the effect of antibiotics and overcome it. Eventually, through the continuous use of the same antibiotic, a group of bacteria that can survive it emerges, originating from these few microbes. Through this process, bacteria is able to withstand the attack of multiple antibiotics, and ‘superbugs’ are born.
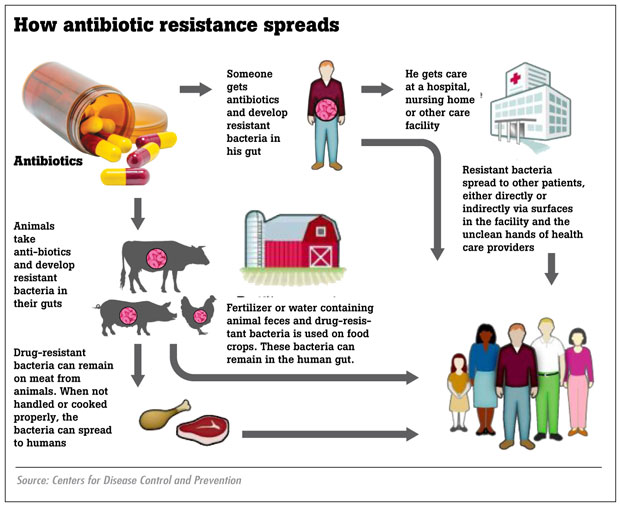
When these mutated species spread from one person to another, these antibiotics will not work on the latter either.
One could suggest that the easiest solution is to find newer antibiotics to compensate for the newly-emerging subgroups but this is practically impossible because despite numerous research and millions of dollars spent, only one new antibiotic has been produced in the last thirty years.
Today, these antibiotic-resistant infections cost a great deal of time and money, with prolonged hospital stays and costly drugs being administered, in addition to isolated treatment in the ward and increasing death rates when compared to normal infections. If this threat continues, higher numbers of antibiotic-resistant bacteria will form and spread and there will come a day when there are groups of disease-spreading ‘superbug’ bacteria which will not respond to even the strongest antibiotics. This will literally take us back to the Middle Ages and will make us incapable of curing even a simple skin infection or a strep throat.
Antibiotic-resistance has always existed but it has been blown out of proportion due to people’s carelessness. Prevention of this fast-growing disaster is the responsibility of both doctors who prescribe antibiotics and patients who use them. Doctors should be cautious to prescribe antibiotics according to the required guidelines, only when it is necessary and to inform patients on the correct use of antibiotics. Special hygienic measures must be taken when treating patients with suspected antibiotic-resistant illnesses in order to avoid spreading the bacteria to another person.
We are accustomed to self-prescribing antibiotics even for small ailments like colds and sore throats. Remember that most of the time, these diseases are caused by viruses which will be cured automatically by the body’s immune system without the help of medication.
Thus, always follow the doctor’s advice on using antibiotics. Never insist on antibiotics if your doctor says you don’t need them. When an antibiotic is prescribed, even if the signs and symptoms of the illness disappear, continue the drug course until the end. Do not use antibiotics leftover from an earlier course for another aliment. Finally, prevention of the spread of infection through improved hygiene is the best method of fighting the war against these little organisms.
23 Dec 2024 8 hours ago
23 Dec 2024 9 hours ago
23 Dec 2024 23 Dec 2024
23 Dec 2024 23 Dec 2024