06 Nov 2020 - 843
 Non-Communicable Diseases (NCDs) are the leading cause for global mortality rates and also responsible for 70% of global deaths. However, due to the COVID-19 outbreak infectious diseases have spiked mortality and morbidity rates across the world. According to new research studies there is an impact of Non-Communicable Diseases on progression and prognosis of infectious diseases such as COVID-19.
Non-Communicable Diseases (NCDs) are the leading cause for global mortality rates and also responsible for 70% of global deaths. However, due to the COVID-19 outbreak infectious diseases have spiked mortality and morbidity rates across the world. According to new research studies there is an impact of Non-Communicable Diseases on progression and prognosis of infectious diseases such as COVID-19.
According to a WHO classification (NCDs are known as chronic diseases and tend to be having a long duration. They result from a combination of genetic, physiological, environmental and behavioral factors. NCDs are non-infectious and non-transmissible among people. There are four (04) main types of NCDs such as cardiovascular diseases (heart attacks and strokes), cancers, chronic respiratory diseases (chronic obstructive pulmonary disease and asthma) and diabetes. The World Health Report 2002 of WHO has indicated that tobacco use, alcohol consumption, being overweight, lack of physical inactivity, high blood pressure and high cholesterol are some vital risk factors associated with NCDs.
COVID-19 predominantly causes respiratory manifestations, including flu-like symptoms and interstitial pneumonia, which may rapidly progress to Acute Respiratory Distress Syndrome. However other organs such as the heart, the liver and the kidneys are also affected and some patients eventually die from multi-organ failure. Initially COVID-19 has been divided into four (04) types: mild, moderate, severe, and critical cases. But with the global outbreak there is increasing evidence to prove that many COVID-19 cases are asymptomatic and the virus in such patients can be transmitted to others.
An asymptomatic COVID-19 infection means that the detection of nucleic acid of SARS-CoV-2 in a sample taken from a patient obtained by Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) is positive. But these patients don’t show typical clinical symptoms or signs.
Different individuals may show different clinical signs. Research studies have shown that asymptomatic infections are more common among young and middle-aged individuals with a functional performance status without underlying diseases. In addition to that a recent study suggests that people who are asymptomatic have a weaker immune response than those who fall sick.
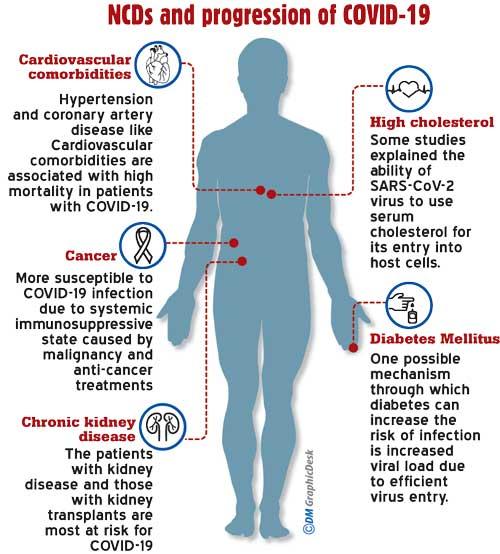
Generally patients with compromised immune systems are considered to be particularly vulnerable to the COVID-19 infection. Most of the previous studies have discovered that among symptomatic individuals hospitalised for COVID-19 old age and presence of some disease conditions such as hypertension, diabetes mellitus, stroke, cancer, kidney issues and high cholesterol are high-risk factors that would have an impact on severity of the COVID-19 disease.
Diabetes mellitus
One possible mechanism through which diabetes can increase the risk of infection is an increased viral load due to an efficient virus entry. This is because the coronavirus uses angiotensin converting enzyme 2 (ACE2) as a receptor for entry into the host and expression of ACE2 is markedly increased in patients with Diabetes Mellitus and hypertension. Therefore, these two disease conditions will facilitate the entry of the coronavirus. And elevated glucose levels may also suppress the antiviral response. In addition to that individuals with diabetes have been said to have alterations in innate immune system components. For example initial cellular events to recognise and kill pathogens such as chemotaxis and phagocytosis are impaired in individuals with diabetes. Glycation of immunoglobulin (glucose molecules attaching to proteins) damages the function of antibodies. Moreover, individuals with (Type 2 diabetes) T2D may have impairments in their alveolar function and earlier studies have shown that pulmonary function parametres such as forced vital capacity, total lung capacity, alveolar membrane permeability, and alveolar gas exchange were significantly reduced in individuals with T2D. Furthermore severe COVID-19 has been associated with a significantly increased risk for developing deep vein thrombosis through activation of coagulation due to profound inflammatory response. Individuals with diabetes are exposed to the increased risk of making more pronounced inflammatory response.
Cancer
Cancer patients are more susceptible to the COVID-19 infection than individuals without cancer. This is because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments such as chemotherapy or surgery.
Cardiovascular comorbidities
Hypertension and coronary artery disease like Cardiovascular comorbidities are associated with high mortality in patients with COVID-19. Drugs are used to reduce cardiovascular risk. Hence drugs such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) have numerous effects that might influence susceptibility to or the severity of COVID-19. Furthermore COVID-19 can also induce cardiovascular manifestations including myocardial injury, myocarditis, arrhythmias, acute coronary syndrome and thromboembolism. Among these cardiovascular manifestations, myocardial injury has been independently associated with high mortality among patients with COVID-19.
Chronic kidney disease
The patients with kidney disease are most at risk of contracting COVID-19. Those with a kidney transplant, due to immunosuppression, and those who receive hemodialysis treatments are exposed to threat due to the inability to self-isolate.
High cholesterol
Some studies have explained about the ability of the SARS-CoV-2 virus to use serum cholesterol for its entry into host cells. And also statin drugs taken for cholesterol control may contribute to the severity of the COVID-19 disease. This is because such drugs by inhibiting endogenous cholesterol, leads to the increased regulation of LDL and this leads to higher membrane cholesterol levels that enhance the ability of SARS-CoV-2 to enter host cells.
According to the above stated factors a person who has NCDs need to pay more attention to NCD management in order to minimise severe risk of COVID-19.
(The writer holds a MSc. Degree in Industrial and Environmental Chemistry from the University of Kelaniya and a BSc in Food Production and a Technology Management degree from the Wayamba University of Sri Lanka)
06 Jan 2025 5 hours ago
06 Jan 2025 5 hours ago
06 Jan 2025 5 hours ago
06 Jan 2025 6 hours ago
06 Jan 2025 6 hours ago