14 Dec 2017 - {{hitsCtrl.values.hits}}
Parkway Cancer Centre’s Dr. Patricia Kho discusses improvements in immunotherapy which can increase the rate of survival for several types of cancer. Immunotherapy is a type of treatment that uses certain parts of a person’s immune system to fight cancer. This works in two ways, one of which is to stimulate the immune system to attack the disease at a cellular level.
Using vaccines is one of the earliest forms of immunotherapy, where a weakened version of bacteria is introduced into the body, so that the immune system can learn how to fight off the actual disease. Immune checkpoint inhibitors, which is the current ground-breaking therapy, releases the ‘brakes’ on one’s immune system and harnessing one’s immune system to recognise and attack the cancer cells.
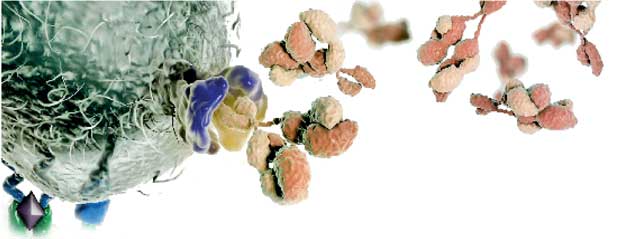
The second way that immunotherapy works is by providing the body with immune system components, such as man-made immune system proteins. The advent of technology, especially in the area of cancer treatment, has allowed for the advancement of immunotherapy where drugs can specifically target cancer cells while leaving healthy cells undamaged.
 Types of immunotherapy
Types of immunotherapy
Immunotherapy drugs are used to treat a wide variety of cancers, including lung, melanoma, head and neck, gastrointestinal, breast, kidney, bladder and Hodgkin’s lymphoma. The main types of immunotherapy used now include monoclonal antibodies, immune checkpoint inhibitors, and cancer vaccines.
The use of immune checkpoint inhibitors to treat cancer could be more effective than chemotherapy or targeted therapy in certain cancers as it has higher response rates with longer disease control periods and has fewer incidences of side effects.
How does immune checkpoint inhibitors work?
Our immune system has checkpoint proteins, such as PD-1. Specifically, it is a checkpoint protein on immune system cells called T-cells and prevents them from attacking healthy cells. It does this when it attaches to a protein called PD-L1. Cancer cells sometimes have large amounts of PD-L1, which help them fool our T-cells into leaving them alone.
PD-1 inhibitors include drugs like Pembrolizumab and Nivolumab. These drugs block the binding of PD-L1 to PD-1 and allow our T-cells to recognise and kill tumour cells. These drugs are administered via intravenous injection, intravesical therapy or applied topically.
Who is suitable for immunotherapy?
This depends on the type of cancer you have. Although it is effective for a wide range of cancers, you may have to undergo other types of therapy before starting on immunotherapy. For example, in non-small cell lung cancer, if your cancer is EGFR mutation-positive, you will require targeted therapy first as it is the most effective for mutation positive non-small cell lung cancer. However, if your cancer is mutation negative, you may benefit from immunotherapy first. Speak to your doctor to determine if immunotherapy can be implemented into your treatment plan.
Side effects and other considerations
Rare immunotherapy does have side effects. These include pneumonitis (inflammation of the lungs), colitis (inflammation of bowels), and endocrine disorders such as thyroid abnormalities and adrenal insufficiency. Fortunately, if side effects are detected early and treated early, most of these side effects can be managed. Hence, it is important that they are administered by experienced oncologists.
23 Dec 2024 1 hours ago
23 Dec 2024 2 hours ago
23 Dec 2024 2 hours ago
23 Dec 2024 3 hours ago
23 Dec 2024 4 hours ago