“Even if there is a single case left, it is adequate to infect millions of children again”
Reported to have paralyzed around 1000 children per day and reporting around 350 000 annual cases, polio was one of the most feared diseases in the 20th century. However, due to the 1988 Global Polio Eradication Initiative, the incidence of polio has been reduced to more than 99%, with polio being endemic in only two countries currently- Pakistan and Afghanistan. Sri Lanka was declared polio-free since 1993 while the WHO South- East Asia region was certified as polio-free in 2014. Recently, WHO Africa Region was declared free of wild-type polio. Even though the incidence of polio remains less than 1%, Dr. Padma Gunaratne, Consultant Neurologist and President- Elect of the Sri Lanka Medical Association, remarked that even with one case, polio is highly infectious.
What is Polio?
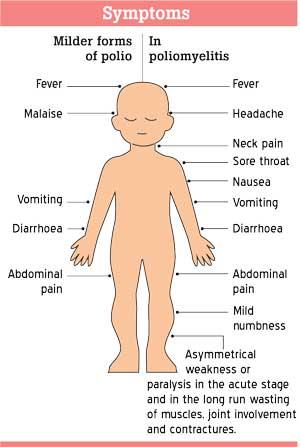
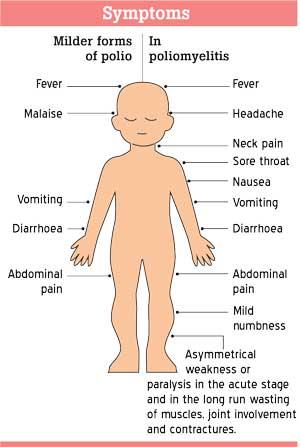
“Poliomyelitis is an acute infectious disease that affects the central nervous system. It generally affects children less than 5 years old. This disease is caused by a RNA virus known as the poliovirus. However, not everyone who contracts the polio virus gets the poliomyelitis disease, only 1 in 200 affected people develop the disease,” stated Dr. Gunaratne. She added that for the milder forms of polio the symptoms are: fever, malaise, diarrhoea, abdominal pain and vomiting. In poliomyelitis, the symptoms are: fever, headache, sore throat, nausea, vomiting, abdominal pain, diarrhoea, neck pain, mild numbness, asymmetrical weakness or paralysis in the acute stage and in the long run wasting of muscles, joint involvement and contractures.
Dr. Gunaratne pointed out various reasons for people to not develop poliomyelitis:
- Type of virus (Wild Poliovirus (WPV) type 1/ WPV type 2/ WPV type 3- the types aren’t equally virulent)
- Load of virus
- Individual factors of the virus
- Individual factors of the environment
- Individual factors of the person (person’s immune system, susceptibility etc.)
“The virus transmits through the faeco-oral route. If a person drinks water contaminated with faecal matter containing poliovirus, the virus gets into the body via the mouth, settles in the throat, multiplies and then spreads via the oral cavity to the intestine and to the nervous system. The virus multiplies in the nerve cells, causing damage and may destroy nerve cells. The virus can cause inflammation of coverings of the nervous system described as viral meninigitis, the spinal cord as myelitis and inflammation of brain as encephalitis.” she explained. Touching on how the poliomyelitis causes paralysis, Dr. Gunaratne shared that the virus multiplies in the anterior horn cells or motor neurone in the spinal cord and damages the cell. “The anterior horn cells are very important for the motor function, therefore damage to it causes paralysis in patients,” she elaborated.
In about 5%-10% of poliomyelitis cases, even respiratory muscles are paralyzed. This resulted in patients’ breathing assisted through assisted ventilation. “In the past, ventilators were not available so iron lungs were used to assist such patients,” revealed Dr. Gunaratne.
She also stated that if patients survived the acute phase of poliomyelitis, they would gradually improve however patients could be crippled for life due to wasting of muscles leading to residual weakness, deformed limbs and joints. “The disease affects limbs asymmetrically. As disease affects the growing limbs of children, the affected limb maybe shorter in height than the other leading to curving of the spine. Therefore, the management of the disease is primarily concerned on rehabilitation,” she remarked.
Dr. Gunaratne also stated that people who have been left with residual disability of limbs following polio for years may start gradual worsening of weakness at 40 -50 years of age. This condition is known as “post polio syndrome’.
Polio success stories credited to the polio vaccine
There are two types of polio vaccines: oral polio vaccine (OPV) and the inactivated polio vaccine (IPV) given as an injection. According to Dr. Gunaratne, OPV is a live vaccine that consists of weakened polio virus and it gives a better community-wide protection against polio. “We use both OPV and IPV in our vaccination regimes. However, the IPV is administered in developed countries to avoid the risks involved with live vaccines,” she said.
Dr. Gunaratne also noted that IPV can cause allergies in individuals who are allergic to its components. “In such cases the OPV is administered, but in most countries that administer IPV, the OPV is not available. However, other than vaccine there aren’t any other alternative method to prevent contraction of the poliovirus,” she said. She noted that after global efforts to administer the polio vaccines globally, the prevalence of the disease dramatically decreased.
Can migration cause polio?
Due to polio being endemically transmitted in two countries which are in close proximity to Sri Lanka, there is a chance of infection via migration. However, Dr. Gunaratne notes that due to the WHO protocol, travellers, especially young children, are vaccinated against polio, resulting in a very small chance of re-emergence of polio via migration.
“In Sri Lanka, the Ministry of Health routinely screens children under the age of 15 years present to hospitals with paralysis, for polio,” revealed Dr. Gunaratne reiterating that maximum effort is taken by authorities locally to eradicate polio and ensure re-emergence of polio is unlikely to occur.

 Reported to have paralyzed around 1000 children per day and reporting around 350 000 annual cases, polio was one of the most feared diseases in the 20th century. However, due to the 1988 Global Polio Eradication Initiative, the incidence of polio has been reduced to more than 99%, with polio being endemic in only two countries currently- Pakistan and Afghanistan. Sri Lanka was declared polio-free since 1993 while the WHO South- East Asia region was certified as polio-free in 2014. Recently, WHO Africa Region was declared free of wild-type polio. Even though the incidence of polio remains less than 1%, Dr. Padma Gunaratne, Consultant Neurologist and President- Elect of the Sri Lanka Medical Association, remarked that even with one case, polio is highly infectious.
Reported to have paralyzed around 1000 children per day and reporting around 350 000 annual cases, polio was one of the most feared diseases in the 20th century. However, due to the 1988 Global Polio Eradication Initiative, the incidence of polio has been reduced to more than 99%, with polio being endemic in only two countries currently- Pakistan and Afghanistan. Sri Lanka was declared polio-free since 1993 while the WHO South- East Asia region was certified as polio-free in 2014. Recently, WHO Africa Region was declared free of wild-type polio. Even though the incidence of polio remains less than 1%, Dr. Padma Gunaratne, Consultant Neurologist and President- Elect of the Sri Lanka Medical Association, remarked that even with one case, polio is highly infectious.