14 Aug 2017 - {{hitsCtrl.values.hits}}

 It’s time to clear the air regarding the little plastic lifesaver-better known as the inhaler- you use. The inhaler is another simple yet invaluable invention of modern medicine. This gadget makes taking treatment for lung conditions less of an encumbrance for both the doctor and the patient. But despite being around for decades, there are still so many misconceptions surrounding inhalers. In addition, a research done in UK has revealed that one in three patients who are using inhalers aren’t using them properly.
It’s time to clear the air regarding the little plastic lifesaver-better known as the inhaler- you use. The inhaler is another simple yet invaluable invention of modern medicine. This gadget makes taking treatment for lung conditions less of an encumbrance for both the doctor and the patient. But despite being around for decades, there are still so many misconceptions surrounding inhalers. In addition, a research done in UK has revealed that one in three patients who are using inhalers aren’t using them properly.
I remember once a consultant physician recalling his experience while being abroad, where an asthmatic patient-whose symptoms hadn’t improved despite the prescribed inhaler- came to him. Yes, she was using the inhaler and twice a day as the doctors recommended. However, when asked to demonstrate how she was using the inhaler, she took out the device and ‘spritz’ ’ spritz’, sprayed the medicinal cloud under her armpits. Even though our readers are much more aware of the medical world behind them, there are so many little things that can go wrong while using the inhaler. There are also the shadows and the myths that need to be brought to light when making references to this topic.We hope this article will be of some use to both the users of inhalers and the ones who were advised to use an inhaler, but are reluctant, due to various reasons.

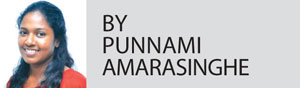
If you are prescribed an inhaler, make sure that the healthcare worker instructs on the correct method of inhaler use before you leave the clinic. Take the device with you on your next visit, so that they can review your method of using the inhaler.
If your inhaler is to be used when you get the symptoms, make sure to keep it with you at all times, because you may need it at the most unexpected time. Following the exact dose that your doctor recommends is essential. If the doctor recommended two puffs, don’t use more than that, because this may cause an overdose of the drug.
When you visit a pharmacy, it has on display inhaler devices that come in various designs and a spectrum of colours.Though the choices are overwhelming, your doctor will help you find the best match for yourself. This is done by considering factors like the severity of the disease, age, occupation and affordability.

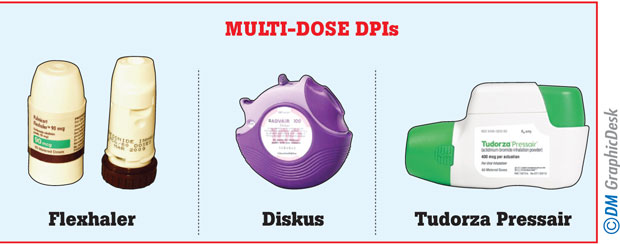
All these fancy gadgets can be divided into two groups. Metered Dose Inhalers (MDI) are the commonest and consist of a canister and a plastic holder. The canister contains the medication with a propellent, which, when pressed, deliveres medication in aerosol form.
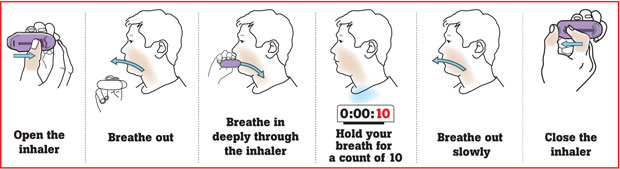
The other group is the Dry Powder Inhaler, otherwise known as the DP-haler. These come in various sizes, shapes and trade names, such as turbohaler, accuhaler, cyclohaler etc. With regard to these, you either have to insert a capsule with the powdered medicine or the device will contain a specific number of doses of medicine. They don’t have a propeller and depend on the force of the patient’s inhalation to get medicine into the lungs.

In cases where the patient is too old or ill or in the case of children, where the above instructions can’t be followed, you will be prescribed a transparent bubble like device called a ‘spacer’ along with the MDI. After attaching the mouthpiece of the inhaler to the spacer device, the drug will be directly delivered to the chamber of the spacer, so you can take smaller more regular puffs of breaths through the mouthpiece of the spacer or through a face mask.

Some are reluctant to use inhalers, preferring to continue with oral drugs, thinking they will get ‘addicted’ to the inhaler. These patients also believe that using the inhaler will make them experience side effects.
Oral medication for a lung condition has to be absorbed from the gut. It’s then only that a small percentage of it will be delivered to the lung via blood.
Therefore the dose of the drug that needs to be given to make a clinical effect is comparatively high, unlike with inhalers, where a smaller dose is needed because the drug is directly delivered to the affected site.
Therefore the side effects are much lower compared to the same medication taken orally. Inhaled drugs also act faster and therefore are more suited in the case of acute asthma attacks.
Inhaler users, whose medications contain steroids, are more liable to get oral thrush. This can be avoided by gargling the mouth well after using the device. Most other side effects are experienced as a result of the drug and not because of the inhaler itself. Children on long term inhaler therapy should be monitored for their growth.
The adults who are on steroids will have an increased risk of osteoporosis among other things and also need monitoring.
Medicine, weather it’s western or ayurvedic, aren’t without side effects. But rather than avoiding taking treatment altogether- for the fear of side effects- it’s essential to find the point of balance where the therapeutic effects of treatment out weight it’s bad effects. If we do this the quality of lives would improve drastically.
23 Dec 2024 2 hours ago
23 Dec 2024 3 hours ago
23 Dec 2024 6 hours ago
23 Dec 2024 7 hours ago