21 Aug 2020 - {{hitsCtrl.values.hits}}
 The heart and the blood vessels are basically the pump and pipes of the complex machine, that is the human body. This intricate plumbing system pumps out blood around the clock, throughout our lifetime to keep all the organs well perfused.
The heart and the blood vessels are basically the pump and pipes of the complex machine, that is the human body. This intricate plumbing system pumps out blood around the clock, throughout our lifetime to keep all the organs well perfused.
The function of all the cells in the human body is fueled by oxygen and other nutrients, and blood is the medium that carries the fuel to the cells, via the arteries, arterioles and capillaries, which are all part of the vascular network. A continuous blood supply of these to all the organs is vital for living.
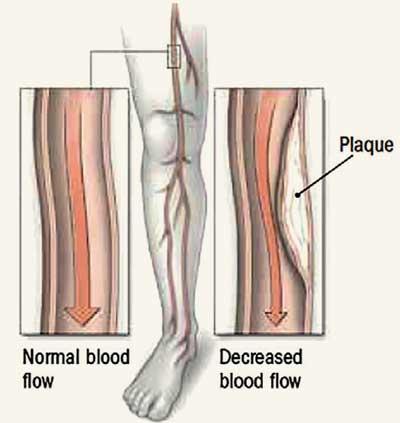
Peripheral Vascular Disease (PVD), also known as Peripheral Arterial Disease (PAD), is a slow and progressive circulation disorder, in which narrowed arteries reduce blood flow to the peripheries, i.e, the limbs. This is a fairly common circulatory problem that may affect any blood vessel outside of the heart and the brain.
Narrowing of blood vessel lumen, caused by either blockage, or spasms in a blood vessel can impede steady blood flow. Blood supply is hence interrupted, and the share of oxygen and nutrients to the area supplied by the affected blood vessels is compromised.
With inadequate blood supply, symptoms gradually arise. Legs and feet are more commonly affected, and the most common symptom of PAD is cramping pain in the lower limbs following exercise, which is relieved by rest. This phenomenon is known as intermittent claudication. While exercising, the demand for oxygen is increased, as the tissues are using up energy. When the diseased blood vessels fail to meet the demands of the fatigued tissue, pain ensues.
Other signs and symptoms include, but are not limited to, changes in the overlying skin, (cold, thin, shiny appearance) weak pulses in the legs and the feet, gangrene (dead tissue due to lack of blood flow) non-healing wounds over pressure points, such as heels or ankles, numbness and heaviness in muscles, burning or aching pain at night while lying flat, commonly in the toe, and reddish-blue discolouration of the extremities.
The most common cause of PVD is atherosclerosis, the buildup of plaque inside the artery wall. Blood clots may form on the artery walls, further decreasing the inner size of the blood vessel and block the supply. Patients with Coronary Artery Disease are at a risk for developing peripheral arterial disease. The male gender, older age groups (>50), post menopausal women, a strong family history of high cholesterol and/or high blood pressure, are all risk factors.
Physical inactivity, Smoking or use of tobacco products, and obesity are among the modifiable risk factors. Those who smoke or have diabetes have the highest risk of complications from PVD because these risk factors also cause impaired blood flow. The ultimate goal for treatment of PVD, is to control the symptoms such as pain, and halt the progression of the disease to lower the risk for heart attack, stroke, and other coexisting complications. Lifestyle changes including regular exercise, proper nutrition, and quitting smoking, need to be implemented to control risk factors.
Medicines to improve blood flow, such as anti-platelet agents (blood thinners) and medicines that relax the blood vessel walls can be prescribed with extensive disease.
Angioplasty and atherectomy are minimally invasive options and vascular surgery is performed in severe cases, where a bypass graft is placed in the area of the blocked or narrowed artery to reroute the blood flow, just like in the better known cardiac bypass surgeries.
Early diagnosis and intervention is of importance, as the affected body part can undergo “ischaemia” due to lack of blood supply, and starts to die. This may even lead to drastic measures like amputation. Prevention is ultimately better than cure.
21 Dec 2024 5 hours ago
21 Dec 2024 7 hours ago
21 Dec 2024 21 Dec 2024
21 Dec 2024 21 Dec 2024
21 Dec 2024 21 Dec 2024