07 Jun 2017 - {{hitsCtrl.values.hits}}

 Sri Lanka faced one of the biggest natural disasters ever in its history with the recent floods, which led to the loss of life of many innocent people. Looking back at these devastating episodes, it is always better to think of how they could have been prevented beforehand so that the negative impact of mother nature could be minimized, while the natural balance of the environment is maintained.
Sri Lanka faced one of the biggest natural disasters ever in its history with the recent floods, which led to the loss of life of many innocent people. Looking back at these devastating episodes, it is always better to think of how they could have been prevented beforehand so that the negative impact of mother nature could be minimized, while the natural balance of the environment is maintained.
The distribution of medical drugs secondary to massive flood relief campaigns are seen throughout the affected areas of the country.
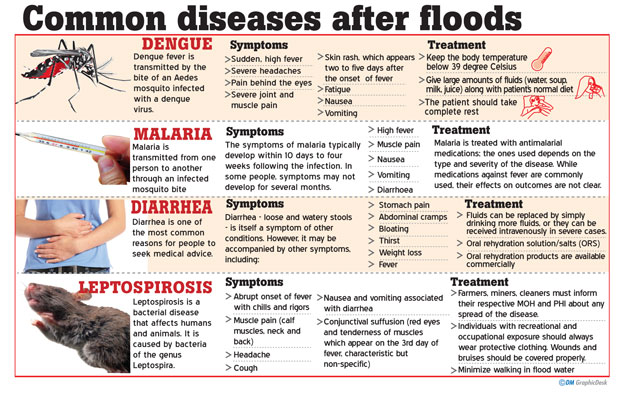
If you have ever taken part in such relief or have listened to the news, Doxycycline is a very common name one hears nowadays. It tops the list of drugs which prevent the disease LEPTOSPIROSIS (Rat fever/ Mee una), a life-threatening illness, most likely to raise its head in the backdrop of heavy freshwater floods.
What is Leptospirosis?
It is a worldwide zoonotic infection where the pathogen is transmitted directly or indirectly from animals to humans. It is commonly observed in tropical and sub-tropical areas of the world. Leptospirosis characteristically peaks during rainy weather or flooding.
Incidence of the condition is higher among paddy farmers and according to the latest data, 3000-5000 people are suspected to be affected every year and many die from the disease (1-2%) if not diagnosed and treated properly.
Other risk groups:
Workers in coconut and sugar cane plantations, abattoirs and fish markets.
In Sri Lanka, suspected Leptospirosis is a notifiable disease and the Matara, Gampaha and Kaluthara areas have recorded the most number of cases in the recent past.

What causes Leptospirosis?
The main causative pathogen is Leptospires, which falls under the phylum of spirochaetes. These are found in the kidneys of animals such as rodents-rats and bandicoots and livestock (cattles, pigs) and wild mammals (rare in Sri Lanka).
Transmission of the infection to humans usually occurs by the exposure of abraded skin or mucous membranes (nasal, oral, eye) to water, wet soil or food and water, contaminated with urine from chronically infected yet asymptomatic animals, especially rodents. Once the pathogen enters the blood stream and invades all the tissues and organs of an individual, the symptoms may appear following 1-2 weeks after the initial exposure, and can occur even before that since the incubation period of the pathogen is found to be 2-26 days (average of 10 days).
How do patients present symptoms?
Leptospirosis is a self-limited systemic infection or a severe, potentially fatal illness accompanied by multi-organ failure.
Initial symptoms (mimic mild flu and Dengue fever)
It is important to be aware of these initial features, in order to seek immediate medical advice before serious complications begin. We have noticed that most patients misinterpret these constitutional symptoms as simple viral fever and tend to ignore them, after which it’s really hard to manage them.
2nd phase
This follows a short period of apparent well-being of the patient and occurs due to body’s immunological response to the infection.
Complications
However, the good news is more than 90% of affected individuals with mild infection will recover spontaneously, even though some may progress up to an increased severity with kidney, heart and liver failure with wide-spread hemorrhage which would ultimately end up in death, if not managed promptly and properly (Case fatality rate -5%-30%: Epidemiological data).
How are the patients diagnosed and managed?
Early diagnosis is crucial in managing patients with Leptospirosis. However, this can be quite challenging due to non-specific initial presentation and difficult lab studies.
Patients with suspected clinical signs and symptoms along with a history of an obvious occupational or recreational exposure should be tested for antibodies in blood and urine which will confirm the diagnosis.
The hallmark of the Leptospirosis treatment is antibiotics.
Suspected patients without any organ involvement or identified co-morbidities can be managed as out-patients and treated with doxycycline-100mg/12 hourly for 7 days.
High-risk patients with organ involvement or co-morbidities should be admitted immediately and treated with antibiotics; Penicillin, Ceftriaxone and Cefotaxime.
What is the importance of Prophylaxis in Leptospirosis?
According to the national guidelines in Sri Lanka, prophylactic treatment for Leptospirosis can only be given under the proper guidance and monitoring of public health authorities. However, during the recent flood crisis, this treatment was highly encouraged in individuals to prevent possible wide-spread of the infection.
-Children under 12 years
-Pregnant and lactating mothers
-Any previous allergic response to the drug Prevention and Control
23 Dec 2024 9 hours ago
23 Dec 2024 23 Dec 2024
23 Dec 2024 23 Dec 2024
23 Dec 2024 23 Dec 2024