05 Apr 2019 - {{hitsCtrl.values.hits}}
 We may come across individuals who claim to have ‘loose’ or ‘double joints,’ but the condition they are actually referring to is hypermobility.
We may come across individuals who claim to have ‘loose’ or ‘double joints,’ but the condition they are actually referring to is hypermobility.
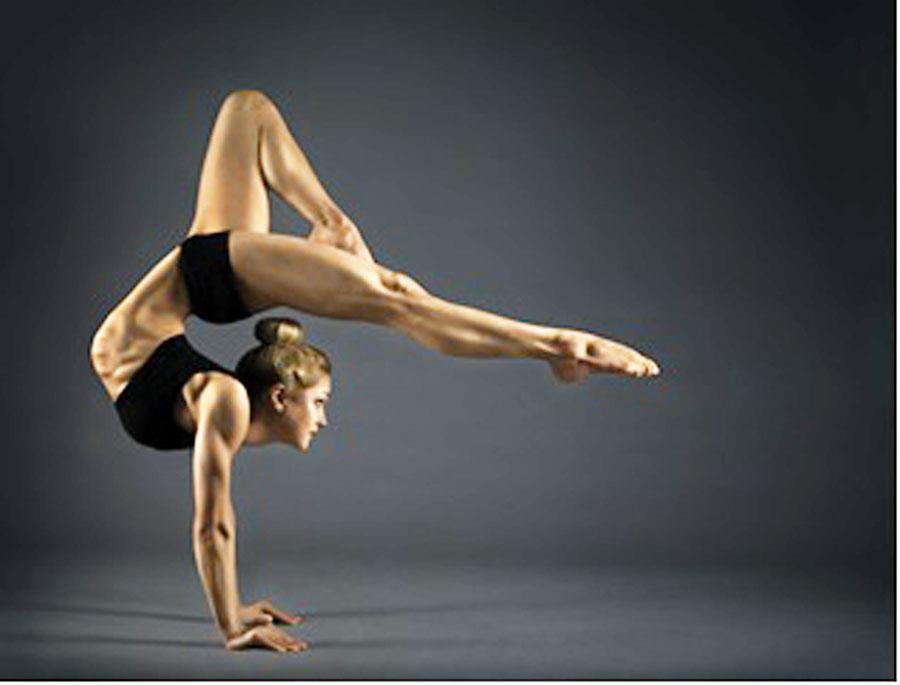
For acrobats, athletes and dancers, being graced with natural hypermobility may be perceived as a major advantage against their less (naturally) flexible competitors. However its precarious side, especially in the long-run and its connection to more serious issues like Ehlers-Danlos or Marfan Syndromes is one that isn’t commonly discussed. Shedding light on all the aspects of Hypermobility, Dr. Himantha Atukorale, Consultant in Rheumatology and Rehabilitation spoke to the
Health Capsule.
Defining Hypermobility
While society most often views this condition as a case of extreme flexibility of certain parts of the body, Dr. Atukorale explained that there’s more to it.
“Hypermobility takes into consideration the joint mobility. That is; how moveable the joints are. There are various reasons as to why the joints move beyond the normal range of movement. Any condition that can cause an excessive movement of joints, we define as a hypermobility syndrome.”
He added that hypermobility considers the “elasticity of the tissues that surround the joint. The area within the joint is healthy, the bones are alright, but somet aspects surrounding the bone including the capsules, the muscles, and the ligaments being elastic can give rise to excessive mobility.”
Causes of Hypermobility
“It could be inherited. There is familial hypermobility syndrome where certain families and their children have hypermobility. This is the commonest cause, but mutations are also possible, where suddenly someone gets it and it cannot be traced back to parents or relatives.”
Dr. Atukorale also mentioned that there are Syndromes associated with hypermobility -such as Marfan or Ehlers-Danlos - usually inherited disorders that are passed on to children by their parents.
Signs and symptoms
According to the American College of Rheumatology, while some children may have no symptoms, others may have joint and muscle pains or mild swelling in the late afternoon or evening or after exercise. These aches and pains are more common in the knees, elbows, and calf and thigh muscles. Symptoms usually improve with rest.
Hypermobile children are more prone to sprains, soft tissue injuries and dislocations of affected joints. Some children may have chronic pain. Others may have loose skin, increased bruising, thin scars and nerve compression disorders.
Growing pains may be more common with hypermobile children. These are cramping or deep, aching pains of the legs, thighs or calf muscles. They typically occur at night and usually are relieved by massage. The involved joints do not tend to have any signs of inflammation like redness or warmth.
Most children become less flexible as they grow older, and their symptoms improve. Rarely, however, symptoms may persist, and a few people are prone to recurrent injuries or dislocations.

Associated risks
While it is common to see children with hypermobility compete seriously in the sporting arena, their temporary edge over the rest may take a turn with time.
“Children with hypermobility may excel in activities like gymnastics, but the long-term outcomes may be disastrous, if they are not properly trained. Excessive training of the body to accept hypermobility may lead to joint instability later on. So they are more prone to joint disease later on in their adulthood,” Dr. Atukorale stated.
“There are serious instances when hypermobility may cause other problems like issues with blood vessel or heart problems. People who have various imbalances in their spine or joints may encounter secondary problems. For example, if someone with hypermobility has an abnormal spinal curvature, this could put pressure on their other healthy structures and cause long-term joint diseases or muscular skeletal pain,” the doctor said.
And as mentioned earlier, there is the possibility that, children may have a more widespread connective tissue disorder associated with their hypermobility such as Marfan or Ehlers-Danlos syndrome.
Diagnosis
Most often, hypermobility is detected and diagnosed when they are children or adolescents. Dr. Atukorale described the use of the Beighton Score System to diagnose hypermobility. This assesses how long the pain has persisted, the symptoms experienced and studies the relevant joints which include toes, ankles, hips and even the neck.
“Some may have only three or four joints with hypermobility, where as other joints are healthy. It is debatable if we should still classify such children as hypermobile, but we still go ahead with physiotherapy and exercises to minimize the symptoms and stabilize the joints,” he explained.
Dr. Atukorale continued that while some people seek medical help as a result of experiencing joint pains and aches, others ( predominantly adolescents) simply discover that they possess hypermobility and consult them with inquiries about the condition. He stressed that early and apt diagnosis is crucial in preventing injuries.
After assessment, the hypermobility may be categorised as mild, moderate or severe. If it is severe, they are given expansive lifestyle modification advice, but if it is mild they are simply directed to physiotherapy.
Treatment of Hypermobility
“There is no proper cure as such for hypermobility, because it affects your connective tissue. This cannot be reversed or changed by administering drugs. If it does persist, the main thing we do is give good advice as what not to do in their adulthood,” Dr. Atukorale expressed.
He added that if a patient with severe hypermobility is engaged in a profession that demands much manual labour, they may be advised to consider a career change in order to avoid many health issues. In addition, even when it comes to sports or fitness, hypermobile people are discouraged from certain activities like weightlifting which might prompt serious spinal problems.
“Pain killers and other tablets don’t usually work. The underlying issue cannot be addressed using painkillers or tablets. Even if it helps in the short-run, in the long run there could be serious side effects from these tablets. So we recommend physical therapy instead,” Dr. Atukorale said.
22 Dec 2024 11 minute ago
22 Dec 2024 2 hours ago
22 Dec 2024 2 hours ago
22 Dec 2024 5 hours ago
22 Dec 2024 5 hours ago