14 Dec 2018 - {{hitsCtrl.values.hits}}

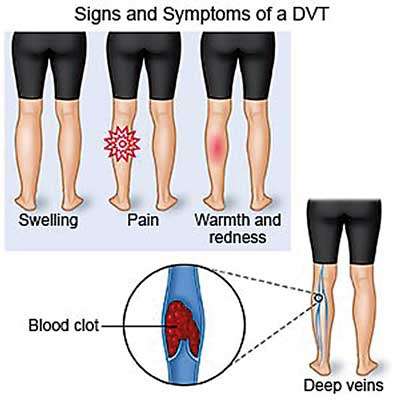
 Ever heard of a medical condition which is caused by a blood clot which lodges inside one of those blood vessels (vein), located deep inside your body and causes one-sided swelling, cramping pain and discomfort on the foot, ankle or calves? Sounds a bit creepy, but yes, there is a condition as such-called Deep Vein Thrombosis.
Ever heard of a medical condition which is caused by a blood clot which lodges inside one of those blood vessels (vein), located deep inside your body and causes one-sided swelling, cramping pain and discomfort on the foot, ankle or calves? Sounds a bit creepy, but yes, there is a condition as such-called Deep Vein Thrombosis.
To shed light on this topic, which is not uncommon and has an incidence of around 1 per 1000 annually in adult populations, we had a discussion with Dr Vindya Wellala, Registrar in Medicine, Teaching Hospital Karapitiya, Galle.
“Often affecting deep veins of the legs, thighs or pelvis, Deep Vein Thrombosis has found to be commonly affecting one’s left leg as a result of the compression of left iliac vein through the right iliac artery” says Dr Wellala. As far as the ‘multifactorial’ causative phenomenon of this condition is concerned medics will be concerned about the following:
People exposed to risk
According to the doctor the risk of DVT is unpredictable- but medics would say that if you are suffering from the conditions mentioned below you are exposed to risk. The conditions:
How patients present with the condition
At certain circumstances they can be associated with other features which are related to systemic disease such as anti-phospholipid syndrome characterised by recurrent miscarriages, migraine like headache.
Many ask whether the pain is felt only the legs? The doctor’s answer is no. “Some people can rarely develop DVT in the upper extremity as well and can present with symptoms including,
“However, the bad news associated with DVT is that some patients would get diagnosed only when they enter hospital due to Pulmonary Embolism- a medical emergency, occurs as a complication of DVT which takes place when a blood clot from the lower extremity, dislodges and places in a blood vessel carrying blood to the lungs. This is why proper awareness about these medical conditions is extremely important, because having few right facts in your head can save lives before they get complicated with unnecessary trouble-even if you are not a health care professional” highlights Dr. Wellala.
The process of getting diagnosed
We can visualise blood vessels via imaging such as compression ultrasonography with Doppler, which is the test of choice when it comes to DVT. This is a test in which a combination of ultrasonography to visualise the vein and Doppler to assess blood flow abnormalities is used.However, there are other options such as,
Once confirmed with DVT we need to look in to the cause such as hypercoagulable state, internal malignancy, unusual site blood clot specially when there is no provocation factor such as immobilization.
Treatment
According to Dr. Wellala it is important to seek immediate medical advice once you notice the first signs and symptoms of DVT as it can give rise to life threatening complications, in the event there is a delay.
Initial treatment usually needs inward care and intravenous or subcutaneous medications to prevent further blood clotting. Meanwhile oral medication will be continued such as warfarin which is a blood thinner.
Lysis of the clot or thrombolytic therapy or removal of the clot by a surgery thrombectomy-used in rare instances in massive proximal DVT. Additionally,
Prevention
Additional food for thought
There are two subtypes of Deep Vein Thrombosis. They are:
This is a severe form of phlebo-thrombosis which is characterised by the obstruction of all veins of one extremity with subsequent compression of arterial flow and high mortality. In this case you will present with severe swelling, oedema and pain on your limbs associated with coldness, cyanosis (bluish discoloration on the area) and pulselessness.
Complications: Shock, gangrene, acute renal failure (due to Rhabdomyolysis)
Treatment is usually an emergency surgery which is venous thrombectomy or fasciotomy where amputation is kept as the last resort. However Fibrinolysis can be considered in case the surgery fails.
This is another form of DVT which is defined as the acute thrombosis of a brachial, axial or subclavian vein. Sometimes called as “Effort-induced thrombosis”, this can be triggered by an extreme activity of the arms during sports, operation of a jackhammer etc. or can be a complication of Thoracic outlet syndrome and lodging a foreign object in veins (central venous catheter, pacemaker lead)
Treatment is usually anticoagulation or fibrinolysis.
Additionally you can develop massive blood clots in your proximal blood vessels which can compress other blood vessels- causing a lack of blood supply to the limb of the affected side, increasing pressure within the limb compartment and causing muscle damage, kidney and impairment. Though it is very rare , it can be a life threatening condition which needs urgent surgery.
22 Dec 2024 21 minute ago
22 Dec 2024 42 minute ago
22 Dec 2024 44 minute ago
22 Dec 2024 5 hours ago
22 Dec 2024 7 hours ago