04 Jan 2019 - {{hitsCtrl.values.hits}}
 A mother brings her child who is only a few days old, to the paediatrician, complaining that the baby is yellow. The doctor finds that the eyes and the skin of the child have indeed turned yellow and requests urgent investigations. Among them are Full Blood Count, Blood Picture and Reticulocyte Count.
A mother brings her child who is only a few days old, to the paediatrician, complaining that the baby is yellow. The doctor finds that the eyes and the skin of the child have indeed turned yellow and requests urgent investigations. Among them are Full Blood Count, Blood Picture and Reticulocyte Count.
Today in Health Capsule we plan to discuss about reticulocyte count, it’s uses and importance, because, even though it is not frequently requested, it is of great importance. Following are excerpts of an interview done with Dr.K.A.C Wickramaratne, Consultant Haematologist and Senior Lecturer in Pathology, Faculty of Medicine, Karapitiya.
Reticulocyte count is reported as a percentage of red cells. However, some laboratories report retic count with some other important additional parameters such as immature fraction, production index which are useful for clinicians but beyond discussion
Q What is Reticulocyte count? What are reticulocytes?
Reticulocytes are young red blood cells. Reticulocyte count is basically the count or quantification of number of reticulocytes present in blood.
Red cells are formed in the bone marrow. New red blood cells are produced and added to your circulation continuously, even while you are reading this.
TRed blood cells (RBCs) can be thought as balloons filled with haemoglobin - the pigment which carry oxygen. These cells are totally devoid of organelles that a normal body cell has.
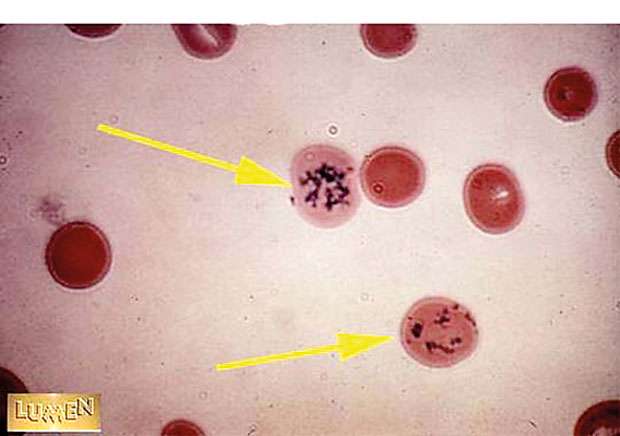
The original mother cells that red blood cells originate from have nuclei and all the sub cellular structures like other cells. These cells loose its nucleus and other structures when they become mature red blood cells. The young and immature red cells with some sub cellular structures retained in the circulation are the reticulocytes. These are not mother cells – as there are no nuclei. They are not completely mature red blood cells either as they have sub cellular structures - few ribosomes and RNAs which are used for the production of haemoglobin. This special property of reticulocytes helps to differentiate them from red blood cells.
Q Why is reticulocyte count requested?
Now we know reticulocytes are the immature red cells. When bone marrow works harder- faster – or to its maximum capacity, we expect release of large number of reticulocytes in to blood. This can happen mainly under two conditions. One is when blood is lost rapidly from the body. We call it “haemorrhage”. The other is when a patient is having a group of disorders called haemolytic anaemia.
In these disorders, red cells are destroyed fast and removed from circulation prematurely, before completion of full life span of a red cell. In haemolysis as well as in haemorrhage, bone marrow produces red cells very fast to supply adequate red cells for body’s demand, releasing a large number of young cells.
Therefore, when haemolysis or haemorrhageis suspected, clinicians request reticulocyte count in which we expect a very high value. The patients with anaemia due to haemolysis or haemorrhage show high reticulocyte counts proportionate to the severity of anaemia.
Normal reticulocyte count is 1-2% in healthy individuals.
On the other hand, there is a group of disorders, we call marrow failure syndromes, in which, marrow cannot produce adequate number of cells. Then we expect less number of reticulocytes. Aplastic anaemia, marrow infiltration etc leads to low reticulocyte count or reticulocytopenia.
Reticulocytes are the immature red cells. When bone marrow works harder- faster – or to its maximum capacity, we expect release of large number of reticulocytes in to blood
Q What are the special instances where Reticulocyte count is useful?
Reticulocyte count and some related test parameters are useful to monitor response to therapy. It may be anaemia due to nutrition deficiency or any haemolytic condition or haemorrhage. Progressive increase of reticulocyte count over first week following treatment is a good indicator of treatment response. Following that, if retic count is declining towards normal count, it means that the haemolysis or haemorrhage is settling.
Cancer treatment causes marrow damage and slows down blood cell production. Reticulocyte count can be used to predict marrow recovery following cancer treatment.
It is a useful marker for monitoring of patients immediately after bone marrow transplant. Rising reticulocyte count indicate successful transplant.
Q What is the sample needed for reticulocyte count?
Venous blood collected any time of the day to a special tube with a chemical called EDTA is used for this test. The EDTA keeps blood in liquid state enabling the test to be performed.
Q What precautions and preparations are needed when blood is collected for retic count?
No special precautions or preparations are needed for reticulocyte count. However, if the test is requested to monitor response to therapy, timing is very important. We should know the baseline retic count value before treatment was started. If the condition being treated for is iron or vitamin B 12 deficiency, performance of retic count within 7th to 10th day since commencement of treatment is the best. This is because over a few weeks following treatment, the retic counts return back to normal values.
Q How should the samples be transported?
Similar to many other tests in haematology, samples collected for retic count should be transported at room temperature (21 – 270 C) within a short period of time to the laboratory. If a delay is expected, refrigeration is needed.
Q How the reticulocyte count is performed and reported?
Most of the laboratories use traditional manual method. If performed appropriately retic count is very reliable. Some laboratories perform fully automated retic count. Retic count test is special since we stain living cells. Fresh liquid blood and staining chemicals are mixed in a test tube and kept for 20 minutes at correct temperature. Finally, a smear is prepared from the well mixed sample with staining chemicals and left for drying.
Dried smear is examined using a microscope to see reticulocytes. Trained and experienced technical personnel or any haematologist can perform counting of retics very accurately.
Reticulocyte count is reported as a percentage of red cells. However, some laboratories report retic count with some other important additional parameters such as immature fraction, production index which are useful for clinicians but beyond discussion here.
Q Can reticulocyte count report be erroneous?
Yes, this can happen if the staining is not good, if sample is clotted or not mixed adequately before testing. The count can also be incorrect if the person who performs the test is inexperienced. The sample quality is very important. The test process too needs meticulous attention. There should be daily quality control and monitoring.
Q Can laboratory perform any other test from the same sample?
Yes. Since, retic count is done using EDTA sample, it can be used for FBC,BP etc. that we have discussed in previous articles.
In summary, reticulocyte count is an important test giving clues on how healthy our bone marrow is. It gives very important information for the clinician for proper diagnosis and monitoring of patients with anaemia. We should always remember that the quality of these test results depend on many factors including collection errors. If you are requesting investigations from outside of hospital, take caution to choose a laboratory with ISO 15189 or CAP accreditation, a qualified team including a haematologist to supervise.
22 Dec 2024 31 minute ago
22 Dec 2024 52 minute ago
22 Dec 2024 54 minute ago
22 Dec 2024 6 hours ago
22 Dec 2024 7 hours ago