05 Apr 2019 - {{hitsCtrl.values.hits}}

 “Of all the self-fulfilling prophecies in our culture the assumption that ageing means decline and poor health is probably the deadliest” says Marilyn Ferguson. Everybody ages, but getting there in the right way at right time can be misinterpreted by most people, re-defining the process of ageing as something deadly and debilitating.
“Of all the self-fulfilling prophecies in our culture the assumption that ageing means decline and poor health is probably the deadliest” says Marilyn Ferguson. Everybody ages, but getting there in the right way at right time can be misinterpreted by most people, re-defining the process of ageing as something deadly and debilitating.
According to the World Health Organization (WHO), healthy ageing “is the process of developing and maintaining the functional ability that enables wellbeing in older age”. Functional ability in simple words is the capabilities that enable all people to be and do what they have reason to value which includes a person’s ability to meet his or her basic needs, learn, grow and make decisions, be mobile, build and maintain relationships and to contribute to society.
Stroke is one of the biggest worries, one can encounter during old age and its after-effects can completely demoralise the affected person as well as the family. The incidence of stroke has risen significantly during the past few decades, probably due to the unaccepted lifestyles of our people. Hence on today’s Health Capsule, we are discussing on this timely topic with input coming from Dr. Prasad Thilakarathna, Registrar in Geriatric Medicine, the National Hospital of Sri Lanka
One of the leading causes of long term disability
“Stroke is a leading cause of long-term disability in Sri Lanka with a prevalence of 10.4/1000 in adults and the fourth leading cause of hospital deaths. One person dies of a stroke every six seconds in the world with the main causative factor being thickening of the blood vessels by a process called Atherosclerosis. The older you are, the higher the chance of getting a stroke due to high blood pressure, diabetes mellitus, high cholesterol levels, smoking, excessive alcohol, obesity and sedentary lifestyle which have been identified as the commonest risk factors” says Dr. Thilakarathna.
Ways of presentation can vary
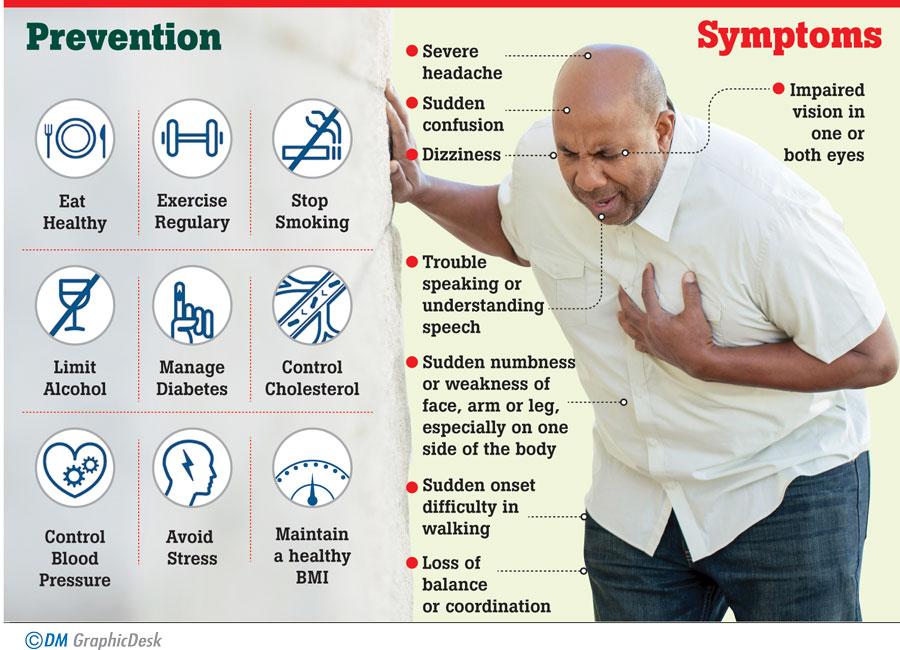
The most common and best known presentations of Stroke include numbness or paralysis of a part or one side of the body. Patients can also present with a sudden change in the vision of one eye or both or inability to speak. Some may even start with a severe splitting headache, dizziness and inability to walk steadily. And in severe cases the patient may become unconscious or end up in sudden death. Early interventions are vital in saving the lives of stroke patients and this is where the importance of knowing about the warning signs comes in handy.
“Sudden numbness or weakness in the face, arm or leg, especially on one side of the body, sudden confusion, trouble in speaking or understanding speech, impaired vision in one or both eyes, sudden onset difficulty in walking, dizziness, loss of balance or coordination, sudden onset severe headache with no known cause are all possible warning signs of impending stroke” explains Dr. Thilakarathna. According to him, the time limit within which the brain tissue can be revived lasts for only 4.5 hours (GOLDEN time) after a blockage, so if you suspect a stroke, note the time at which it happened and bring the patient to the nearest hospital as quickly as possible. More importantly, never ever make attempts to give the patient food or liquids as they may have impaired swallowing which can lead to aspiration.
Golden period
“Once the patient is brought to the hospital, we immediately get a background history of the situation along with patient’s underlying illnesses which must have predisposed to the condition following which a CT scan of the brain is carried out in order to differentiate a haemorrhagic stroke from an ischemic stroke. This differentiation is extremely important as the rest of the management plan would depend on the type of the stroke. Once a hemorrhage is ruled out antiplatelet drugs like Aspirin and Clopidogrel are recommended as blood thinners to prevent clotting. ‘Clot buster’ is an injection given to remove the offending blood clot by dissolving and it is only given within 4.5 hours from the onset of symptoms” the doctor said.
The commencement of early physiotherapy, prevention of pneumonia, pressure sores and clot formation in the leg veins, swallowing assessment and speech therapy are also included in the care of a stroke patient. In simple terms, once the immediate threat to the patient is reversed, our next objective would be to take the patient back to his former lifestyle yet with an improved pattern of living and satisfactory quality of life.
Getting over negativities
Usually following stroke and paralysis, the mobility of a patient is affected adversely (inability to walk, move arms) with the weight of the paralyzed arm on the shoulder causing shoulder pain, immobility of the legs leading to clot formation within the leg veins and body weight on pressure points leading to pressure sores. Furthermore, difficulties in communication, problems in vision and speech, swallowing problems, and loss of bladder and bowel control can also present following stroke in addition to depression, family issues and sexual problems, social issues and economical issues which may arise as long-term consequences. This is why a multi-disciplinary approach is vital when it comes to this kind of pathologies which gives rise to a range of mal-functional aspects of life.
Recovery
“Many people we encounter during our clinical practice pose the question whether a patient can fully recover after a stroke? The answer is “yes”, if the patient reaches a treatment facility within the window period -which is within 4.5 hours- after the onset of symptoms and receives appropriate treatment. However the recovery rate can vary depending on the area of the brain involved, severity of the stroke and care received during the acute and post stroke period. Nevertheless the patient’s motivation and family support play a key role” underscores Dr. Thilakarathna.
Prevention
According to him, getting adhered to a healthy diet, low in saturated fats and sugar, regular exercise, limiting alcohol, abstaining from smoking, stress management and maintaining a healthy BMI (Body mass index) are vital in prevention of strokes. Controlling high blood pressure, cholesterol level and diabetes is also essential in spreading awareness regarding stroke symptoms and the importance of seeking immediate medical care. Even if symptoms settle, these procedures will definitely support in minimizing the complications.
Advances in treatment
“Mechanical thrombectomy is the latest technique employed in the management of stroke, where a device is used to suck out or grab the offending clot from the target vessel. The patient can be treated up to 24 hours from the onset of the stroke using this modality. Catheter directed administration of the thrombolytic agent (“clot buster”) directly on to the clot is also a novel option” highlights Dr. Thilakarathna.
Mini-stroke or “Transient ischemic attack” (TIA)
“This was earlier described as a sudden onset of focal neurological symptoms or signs lasting less than 24 hours. However, the latest definition of TIA is a transient neurological dysfunction without acute brain infarction (tissue injury) where there is no cell death and the patient recovers fully without a residual weakness. “Mini stroke” is a minor form of stroke which creates a slight numbness on one part of the body without any disabling neurological deficit like impaired vision, speech or paralysis of dominant hand. However both forms are associated with increased risk of recurrent strokes” he said.
Take home message
Stroke is a leading cause of long-term disability, adversely affecting one’s physical, mental and economical well-being.
Time is vital in the management of stroke, which is why knowledge of early symptoms is essential.
Prompt initiation of treatment can result in minimal disabilities.
Stroke can be prevented by adhering to a healthy lifestyle and optimizing co-morbidities.
22 Dec 2024 31 minute ago
22 Dec 2024 2 hours ago
22 Dec 2024 2 hours ago
22 Dec 2024 5 hours ago
22 Dec 2024 5 hours ago