23 Feb 2017 - {{hitsCtrl.values.hits}}
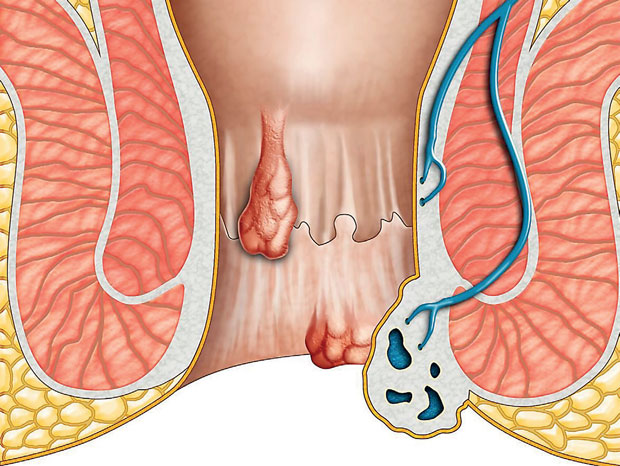
 The digestive system of our body is adapted to break down food and absorb nutrients into our body. The food we swallow travels through the tract and at the end of a 30 foot journey, the unabsorbed food remnants are expelled from our body as stools or faeces. The wall of the bowels form sphincters (valves) that serve as gateways to passage of food particles. The anal canal, the lattermost part of the digestive tract has two such valves, namely the external and internal anal sphincters that aid in continence (stool control). In addition, the mucosa and submucosa of the anal canal forms 3 anal cushions that serve as an efficient fluid and gas-proof seal. These cushions are highly vascular structures covered by a thin epithelium. Due to many reasons, these anal cushions may become enlarged, giving rise to the condition known as haemorrhoids or piles. These enlarged, congested cushions often bleed and you will have to seek medical attention immediately.
The digestive system of our body is adapted to break down food and absorb nutrients into our body. The food we swallow travels through the tract and at the end of a 30 foot journey, the unabsorbed food remnants are expelled from our body as stools or faeces. The wall of the bowels form sphincters (valves) that serve as gateways to passage of food particles. The anal canal, the lattermost part of the digestive tract has two such valves, namely the external and internal anal sphincters that aid in continence (stool control). In addition, the mucosa and submucosa of the anal canal forms 3 anal cushions that serve as an efficient fluid and gas-proof seal. These cushions are highly vascular structures covered by a thin epithelium. Due to many reasons, these anal cushions may become enlarged, giving rise to the condition known as haemorrhoids or piles. These enlarged, congested cushions often bleed and you will have to seek medical attention immediately.
Haemorrhoids is a Latin term derived from the Greek word haimorrhois (haima-blood, rhoos-flowing). In our community, most people refer to any abnormal lump or skin tag felt at the anus as “piles”. It is important to know that a lump at the anus or bleeding with defecation does not always mean that you are suffering from haemorrhoids. Lumps may also occur in a more serious conditions such as cancer (colorectal carcinoma), prolapsed rectum (protrusion of the rectum through the anal orifice) andinflammatory bowel disease as well non-threatening isolated skin tags. Consultation of a general surgeon once you experience the symptoms will help timely diagnosis, exclusion of colorectal cancer and apt treatment.
Symptoms
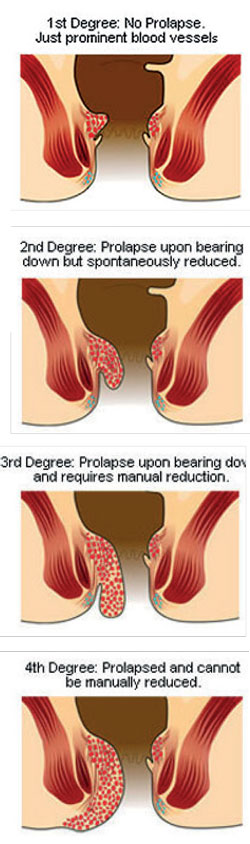
Uncomplicated haemorrhoids are usually associated with painless bleeding with defecation (passage of stools). Blood appears bright red on toilet paper or may splash on to the lavatory pan if the bleeding is heavy. The second symptom is a lump felt in the anus, following defecation and haemorrhoids are classified into 4 types accordingly.
First degree - No prolapse felt (lump). Only bleeding
Second degree - Piles prolapse but reduce spontaneously
Third degree - Piles prolapse. Reduction has to be done manually
Fourth degree – Piles permanently prolapsed
In addition
These symptoms may vary with the individual’s diet, physical activity and psychological stress levels.
What causes haemorrhoids?
The current understanding of it reveals that shearing forces exerted on the anus cause mucosal trauma and the downward displacement of these anal cushions distorting the supporting structures lead to a loss of elasticity (the ability of an object to resume its normal shape after being stretched), that causes failure to retract following defecation. The shearing forces are generated as a result of the following.
Haemorrhoids may occur in any age group but are extremely rare in children. It is uncommon in individuals below the age of 30, although women in that age category may develop it during pregnancy or after childbirth.
Although both sexes are affected, there’s a slightly higher incidence in men than in women. The occurrence in children is extremely rare. 10 percent of the population experience symptomatic haemorrhoids at some point of their lives. It is found to be more prevalent in urban areas compared to rural and more in those with a higher socio-economic status, that may be a result of dietary deficiency of fibre. They are more common in individuals with raised abdominal pressure (i.e. constipation, pregnancy, obesity).
This condition has periods of relapse and spontaneous resolution that may cause delayed presentation for medical help. Some are reluctant to seek help as they find this condition mortifying. This is a benign disease condition that is often repressed by the affected, fostering a significant negative impact on their lives, as it causes constant physical and psychological discomfort, such as lack of self-esteem and poor educational/work performance. The pain during defecation makes the individual reluctant to pass stools that further precipitates the condition. Early detection and treatment avoids complications and relieves discomfort.
Complications
Diagnosis
The diagnosis of haemorrhoids is made by a clinician based on the symptoms and a digital rectal examination findings. In addition a proctoscopy (the proctoscope is an apparatus that helps view the anal cavity) is performed. The possibility of colorectal cancer should always be excluded with performance of a sigmoidoscopy or colonoscopy. A small percentage of haemorrhoids are associated with colorectal cancer.
Management
The classification into different degrees helps decide on the management plan. The initial intervention consists of conservative treatments for those with first and second degree haemorrhoids. Conservative measures include adding wholegrain bread and cereals (wheat, oats barley and rye) , fruits, vegetables, nuts and legumes softens and increases the bulk of stools allowing easier and less strenuous passage owing to the high dietary fibre content (A daily minimum of 25g fibre for women and 38g for men is recommended) An adequate amount of water (at least 8 glasses per day) complements the high fibre diet. In addition, stool softeners and bulking agents, evacuation of bowels only when nature calls and adaptation of defecating positions help minimize straining. Suppositories and various topical creams may alleviate symptoms.
If first and second degree haemorrhoids do not improve with conservative measures, the surgeon proceeds with other non-operative interventions such as sclerotherapy injections. For bigger piles, ‘banding’ is a less common method used. Third and fourth degree piles, second degree piles that do not respond to non-operative measures, complicated external piles or severe bleeding causing anaemia require surgical interventions such as haemorrhoidectomy. Haemorrhoids are a benign condition resolved with prompt medical care. It is important to seek help as soon as possible, to nip it in the bud and avoid complications. Since prevention is always better than cure, be mindful to incorporate high dietary fibre in meals, drink plenty of water, exercise moderately to increase the basal metabolic rate of the body, avoid prolonged sitting on the toilet and initiate defecation only when you have the urge and avoid straining.
25 Dec 2024 34 minute ago
25 Dec 2024 40 minute ago
25 Dec 2024 50 minute ago
25 Dec 2024 1 hours ago
25 Dec 2024 3 hours ago