16 Mar 2018 - {{hitsCtrl.values.hits}}
 Patients with a variety of medical disorders consult General (Internal) Physicians with various symptoms and signs. Swelling of legs is a very common symptom and a sign observed in clinical practice. A large number of conditions can cause swelling in the legs. Common causes of swelling in the legs are cirrhosis (chronic liver cell disease), chronic kidney disease, congestive heart failure, hypothyroidism, nephrotic syndrome and malnutrition. In some patients it’s not possible to find a definitive cause.
Patients with a variety of medical disorders consult General (Internal) Physicians with various symptoms and signs. Swelling of legs is a very common symptom and a sign observed in clinical practice. A large number of conditions can cause swelling in the legs. Common causes of swelling in the legs are cirrhosis (chronic liver cell disease), chronic kidney disease, congestive heart failure, hypothyroidism, nephrotic syndrome and malnutrition. In some patients it’s not possible to find a definitive cause.
Cirrhosis is a common cause for swelling in the legs. Cirrhosis is a very common condition and is the fourteenth most common cause of death globally. In Europe cirrhosis is the 4th most common cause of death. At the time of the presentation to clinicians, most patients are in the advanced stage of the disease. Many patients die from this disease in their fifth or sixth decade of life.
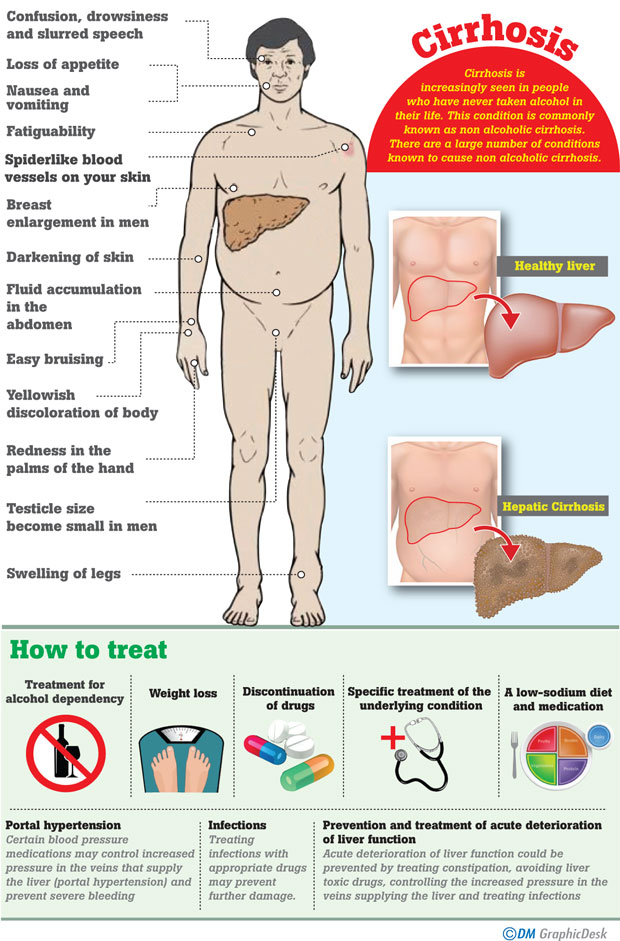
Cirrhosis can be caused by a large of number of conditions. Globally alcoholic liver disease is considered to be the most common cause of cirrhosis. Cirrhosis is increasingly seen in people who have never taken alcohol in their life. This condition is commonly known as non alcoholic cirrhosis. There are a large number of conditions known to cause non alcoholic cirrhosis.
Definition 
Cirrhosis represents a late stage of progressive hepatic fibrosis with distortion of the hepatic architecture and the formation of regenerative nodules. It is irreversible in its advanced stages and needs liver transplantation as the treatment.
What are the signs and symptoms?
Cirrhosis often has no signs or symptoms until liver damage is extensive. When signs and symptoms do occur, they may include:

What are the causes of non alcoholic cirrhosis?
How is cirrhosis diagnosed?
In the advanced stage, with symptoms and signs mentioned above, cirrhosis can be diagnosed clinically.
In early stage of the disease and to confirm the diagnosis following investigations are needed.
Aminotransferases – Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are usually moderately elevated in patients with cirrhosis.
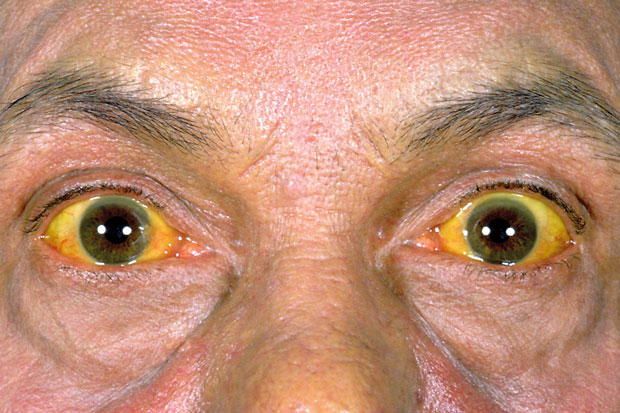
Bilirubin – Bilirubin levels may be normal in well-compensated cirrhosis. However, they rise as the cirrhosis progresses.
Albumin – Albumin is synthesized exclusively in the liver. Albumin levels fall as the synthetic function of the liver declines with worsening cirrhosis. Thus, serum albumin levels can be used to help grade the severity of cirrhosis.
Prothrombin time - The prothrombin time increases as the ability of a cirrhotic liver to synthesize clotting factors diminishes.
Alkaline phosphatase – Alkaline phosphatase is usually elevated in the setting of cirrhosis, but is less than two to three times the upper normal limit.
Platelet count – A low platelet count (thrombocytopenia) is common. Thrombocytopenia is mainly caused by portal hypertension with attendant congestive splenomegaly.
Haemoglobin level – A low haemoglobin level (anaemia) is usually multifactorial in origin; acute and chronic gastrointestinal blood loss, folate deficiency, direct toxicity due to alcohol.
Ultrasound Scan – Ultrasound Scan is routinely used during the evaluation of cirrhosis. It is noninvasive, well tolerated, widely available, and provides valuable information. In advanced cirrhosis, the liver may appear small and nodular. Surface nodularity and increased echogenicity with irregular appearing areas are consistent with cirrhosis.
Liver biopsy — The gold standard for diagnosing cirrhosis is examination of an explanted liver, either at autopsy or following liver transplantation, because the architecture of the entire liver can be appreciated. In clinical practice liver biopsy is performed to see the liver histology. However, liver biopsy is not necessary if the clinical, laboratory, and radiologic data strongly suggest the presence of cirrhosis and if the results would not alter the patient’s management.
What are the complications of cirrhosis?
How to treat cirrhosis?
The goals of treatment are to slow the progression of scar tissue in the liver and to prevent or treat symptoms and complications of cirrhosis. If diagnosed early it may be possible to minimize damage to the liver by treating the underlying cause.
Treatment for alcohol dependency
People with cirrhosis caused by alcohol abuse should stop drinking.
It is essential to stop drinking since any amount of alcohol is toxic to the liver.
People with cirrhosis caused by nonalcoholic fatty liver disease may become healthier if they lose weight and control their blood sugar levels.
If cirrhosis is caused by some drugs, they should be discontinued immediately.
Medications may limit further damage to liver cells caused by hepatitis B or C through specific treatment of these viruses.
If cirrhosis is due to a condition like Wilson’s disease , treating this condition with specific drugs may retard the progression
A low-sodium diet and medication to prevent fluid buildup in the body may help control fluid in the abdomen (ascites) and swelling
Certain blood pressure medications may control increased pressure in the veins that supply the liver (portal hypertension) and prevent severe bleeding.
Treating infections with appropriate drugs may prevent further damage.
Acute deterioration of liver function could be prevented by treating constipation, avoiding liver toxic drugs, controlling the increased pressure in the veins supplying the liver and treating infections
In advanced cases of cirrhosis, when the liver ceases to function, a liver transplant may be the only treatment option.
(Our source person is Prof. Thilak Jayalath, a Professor in Medicine and Consultant Physician attached to the Professorial Medical Unit of the Teaching Hospital in Peradeniya)
22 Dec 2024 8 hours ago
22 Dec 2024 8 hours ago
22 Dec 2024 22 Dec 2024
22 Dec 2024 22 Dec 2024
22 Dec 2024 22 Dec 2024