06 Sep 2019 - {{hitsCtrl.values.hits}}
Migraine is more than just a headache

 Headache disorders are one of the most common disorders of the nervous system. A headache is not only painful, but it is also disabling, imposing a burden on sufferers that impairs their quality of life and impacting finances negatively. Recurring headaches and the apprehension it causes can damage family and social life and employment. Migraine headaches are the most common headache disorder.
Headache disorders are one of the most common disorders of the nervous system. A headache is not only painful, but it is also disabling, imposing a burden on sufferers that impairs their quality of life and impacting finances negatively. Recurring headaches and the apprehension it causes can damage family and social life and employment. Migraine headaches are the most common headache disorder.
What is a migraine?
According to the International Headache Society (IHS), migraine which is a primary headache disorder, is characterised by long standing symptoms with recurrent headaches. There could be severe attacks of head pain, nausea, vomiting, dizziness, vertigo, and sensitivity to light, sound, and touch. If the headache occurs on 15 or more days a month for more than three months, which, on at least eight days a month, has the features of migraine headache, then it would be a chronic migraine. Occasionally, migraine can also be associated with other diseases such as stroke, heart disease, epilepsy, depression.
The Health Capsule spoke to Dr. Padma Gunaratne, Consultant Neurologist and President of the Sri Lanka Association of Geriatric Medicine to shed light on the topic.
Four stages of a migraine
 According to Dr. Gunaratne, the four stages prevalent in a migraine attack are as follows:
According to Dr. Gunaratne, the four stages prevalent in a migraine attack are as follows:
Prodromal stage: Prodromal symptoms can begin hours or a day or two before the other symptoms of a migraine attack (with/without aura). They include combinations of fatigue, difficulty in concentrating, stiffness in the neck, sensitivity to light and/or sound, nausea, blurred vision, constant yawning, pallor, mood swings, constipation and a dull headache.
Aura: This occurs immediately before or during the attack and can act as a warning of an imminent attack. Dr. Padma identified it as a positive phenomenon, of which the most common symptoms are visual in nature, such as flashing lights, zigzag lines and blurry vision. The next type of aura are sensory disturbances with symptoms such as pins and needles that moves slowly from the place of origin and affects one side of the body, face or tongue. While numbness can follow this sensation, it is a separately occurring symptom. This stage can merge with the headache.
Headache phase: The pain is felt in the front area of the head or on one side of the head. It is generally a throbbing, beating or pulsating type of pain and can be accompanied by nausea and vomiting. The attack can last from 24-72 hours. The place of the headache can vary from attack to attack. Some people also develop photophobia (sensitivity to light) and phonophobia (sensitivity to loud sound) during the attack. Such people would not want to be in a place that has strong lighting and/or in noisy and crowded places.
Postdrome: Symptoms most commonly include feeling tired or weary, difficulty in concentration and neck stiffness, which may follow the resolution of the headache persisting for up to 48 hours. According to the ICHD this area is less well studied.
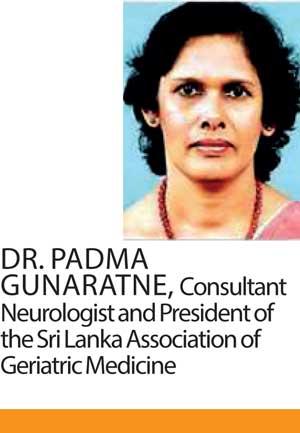
Making lifestyle changes are important for a person who suffers from migraine attacks
Triggers and causes of migraine attacks
“The trigger varies from individual to individual, and there are many types of triggers that are known to bring on migraine attacks,” Dr. Gunaratne said. Certain food items such as, marmite, chocolate, carbonated drinks, peanuts, caffeine and other factors such as, stress, anxiety, hormonal changes in women, inadequate or excess sleep, sudden changes in weather and environment, bright lights, skipped meals, physical overexertion, hormone controlling tablets such as oral contraceptive pills and medication are among the identified triggers for migraine attacks.
“In our clinical practice we see people developing the attacks with fasting, dehydration, menstrual cycles, bathing at certain times, breaking rest and in stressful situations,” observed Dr. Gunaratne.
Dr. Gunaratne stated that many triggers occurring at the same time, carries the highest risk of getting a migraine.
“For example, a person who has broken rest in the night, skipped breakfast and travels without sufficient consumption of water, will invariably be left with a migraine”.
It is important to identify what triggers migraine attacks in order for preventive measures to be taken. Once the triggers have been identified precautions should be taken to avoid several triggers happening simultaneously. “A person should plan their day, as this is important for the management of migraine attacks. Sound sleep, eating meals on time, staying well hydrated and taking on only the amount of work you can cope with, will help to prevent the attacks,” Dr. Gunaratne recommended.
She cautioned against presuming that any severe headache is a migraine attack, when other serious symptoms such as fever and vomiting accompany the headache, especially if the severity and frequency of the symptoms worsen.
Did you know?
Headache disorder is the second leading cause of disability globally (which mainly include migraine), according to the 2017 Global Burden of Disease Study.
According to WHO statistics, adults with a current headache disorder (symptomatic at least once within the last year) is about 50%.
Half to three quarters of adults aged 18–65 years in the world have had a headache in the last year and 30% or more of those individuals have reported migraine.
1.7-4% of the world’s adult population suffer from headaches for 15 or more days every month. Although there might be regional differences, it is a worldwide problem that affects people of all races and ages.
The International Classification of Headache Disorders (ICHD) provides a framework for the diagnosis and treatment of headache which is compiled and published by the International Headache Society (IHS).
Who is at risk of developing migraines?
Dr. Gunaratne revealed that, the migraine headache is generally seen most often in females. “The proportion of females to males is about 8:1. You get it at a young age and it can continue happening on and off”. Those with a family history of migraines are also likely to suffer from migraine attacks.
Treatment
While there is no specific cure for migraines, there is effective medication to treat migraine headaches. “It is important to consider the history of the patients and then proceed to examine them before diagnosing the disorder,” Dr. Gunaratne added. “Either a CT or MRI scan of the brain of the patients, would be required depending on the symptoms they exhibit and the history of the patient,” said Dr. Gunaratne.
The frequency, duration, character, severity, location, quality, and triggering, aggravating, and alleviating features of the headache, should be considered. Dr. Gunaratne revealed, there were two forms of treatment. Treatment to prevent an attack and treatment which focuses on relieving symptoms. “If it is a mild headache, a simple painkiller such as paracetamol would be sufficient. Nonsteroidal anti-inflammatory drugs (NSAID) and an antiemetic drug can be prescribed if symptoms such as nausea and vomiting are prevalent,” advices the Doctor. These are non-specific treatments for migraine.
There are specific drugs for migraine attacks. For severe and acute attacks, Dr. Gunaratne recommends triptan drugs, available in the form of injections (unavailable in Sri Lanka), tablets and nasal sprays. Beta blockers, anti-depressants and anti-epileptic drugs are prescribed as preventive drugs. “We select the drugs based on the profile of the patient and the side effect profile of the drugs, to consider what will be most suitable for the patient,” she said.
Things to do during a migraine,
>Resting with your eyes closed in a quiet, darkened room.
>Placing a cool cloth or ice pack on your forehead.
Drinking fluids
Making lifestyle changes are important for a person who suffers from migraine attacks. Stress management strategies such as exercise, relaxation techniques and a healthy diet can help in reducing the frequency of the attacks. Identify what acts as a trigger for the headache and create a log, listing the triggers and the frequency of the headaches. This would act as reminder of what should and shouldn’t be done. Taking care of oneself on a daily basis and being aware of personal needs will help in reducing migraine attacks. A doctor should be consulted if a headache is recurring and it isn’t advisable to self-medicate.
21 Dec 2024 21 Dec 2024
21 Dec 2024 21 Dec 2024
21 Dec 2024 21 Dec 2024
21 Dec 2024 21 Dec 2024
21 Dec 2024 21 Dec 2024