05 May 2021 - {{hitsCtrl.values.hits}}

One of the challenges Sri Lanka faces is that the majority of the population hasn’t done PCR or Antigen Tests(AFP)
- According to PHI Union President Upul Rohana with the isolation of areas and with less people gathering in towns and public places the situation has somewhat been controlled
- Bed capacity, ambulance services challenged
- Experts say technical and administrative issues may ease spread of virus
- Medical experts opine that herd immunity cannot be achieved by AstraZeneca vaccine
- Non-essential admissions to hospitals declined
- Questions raised on sensitivity, capacity and quality of PCR tests
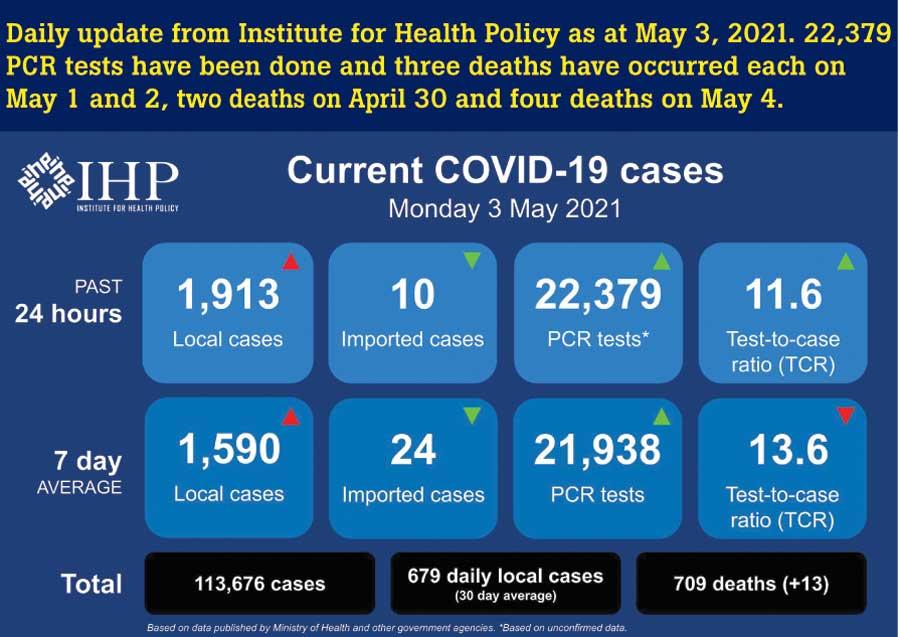
The daily number of cases testing positive for COVID-19 in Sri Lanka is nearing 2000. This is a worrying figure given the numbers that were reported during the first and second waves. While many anticipate that Sri Lanka is heading towards a crisis like that of neighboring India, health officials are challenged with controlling the situation. As more asymptomatic cases are being detected health officials opine that all infected persons should be isolated from the society. But with bed capacity reaching a maximum and with limited ambulance services and limited PCR testing kits, Sri Lanka needs to revisit existing strategies if it is to control this more virulent and deadly strain.
given the numbers that were reported during the first and second waves. While many anticipate that Sri Lanka is heading towards a crisis like that of neighboring India, health officials are challenged with controlling the situation. As more asymptomatic cases are being detected health officials opine that all infected persons should be isolated from the society. But with bed capacity reaching a maximum and with limited ambulance services and limited PCR testing kits, Sri Lanka needs to revisit existing strategies if it is to control this more virulent and deadly strain.
 “The strategy is to isolate any infected person from society” - Dr. Sudath Samaraweera
“The strategy is to isolate any infected person from society” - Dr. Sudath Samaraweera
With over 1500 COVID-19 positive cases being reported for the fourth consecutive day, concerns have been raised on existing facilities in the country. Speaking to the Daily Mirror, Chief Epidemiologist Dr. Sudath Samaraweera said that the strategy is to isolate any infected person from the society. Given below are excerpts of an interview done with Dr. Samaraweera:
Q Are the number of cases testing positive daily related to results of PCR tests or Rapid Antigen Tests?
The majority are from PCR tests.
Q What is the status of facilities for non-COVID patients? Have they been compromised to accommodate more space for COVID patients?
That is obvious. We aren’t taking non-essential admissions.
Q Is there a home quarantine option for asymptomatic patients ?
No. The strategy is to isolate any infected person from society. Therefore they would be sent to a hospital or an intermediate COVID treatment centre.
Another issue is the dearth of ambulances. Apart from that, prior to taking a patient to a hospital or a medical facility they need to be prepared for their stay. So all these matters are time-consuming and sometimes patients have to wait for a day or two prior to getting admitted - PHI Union President Upul Rohana
Waiting lists getting longer
The Public Health Inspectors are vested with the task of moving COVID patients to treatment facilities. Prior to the New Year the PHI Union warned that there could be a surge in the number of cases. However PHI Union President Upul Rohana said that with the isolation of areas and with less people gathering in towns and public places the situation has somewhat been controlled.
However several incidents of COVID positive patients having to return home due to lack of beds were reported. Commenting on the situation Rohana said that some patients have to wait until beds are vacant. “Another issue is the dearth of ambulances. Apart from that, prior to taking a patient to a hospital or a medical facility they need to be prepared for their stay. So all these matters are time-consuming and sometimes patients have to wait for a day or two prior to getting admitted,” said Rohana.
He further said that when a COVID positive patient is detected the individual’s immediate contacts are being informed and are requested to quarantine themselves. “One of the challenges is that the majority of the population hasn’t done PCR or Antigen Tests. Therefore there’s a high possibility of them spreading the disease further,” he warned.
The medical community had enough information to predict all of this two months ago. So did MOH and the Government. In my view this is a scandal as bad as ignoring the intelligence on the Easter Bombings. The only difference is that B.1.1.7 may end up killing more Sri Lankans than the terrorists - Dr. Ravindra Rannan-Eliya, International Medical Researcher and Director at Institute for Health Policy
Cannot have normality with B.1.1.7 variant
When medical experts from Sri Jayawardenapura University (SJU) identified the strain as a more virulent strain of the B.1.1.7 variant, Dr. Ravindra Rannan-Eliya, International Medical Researcher and Director at Institute for Health Policy, took to his Twitter feed claiming that the AstraZeneca (AZ) vaccine may not be good enough to achieve herd immunity. “My understanding of what SJU has said is that B.1.1.7 was in most cases in their April samples. This was expected, but it also means that B.1.1.7 will become almost 100% of the epidemic very soon. In UK it took about 2-3 months, and similarly in other countries.” opined Dr. Rannan-Eliya.
“The latest estimates are that B.1.1.7 is 43-90% more infectious than the preceding global variants. Herd immunity means that the effective transmissibility of the virus in the community falls below 1 without any interventions. With herd immunity we don’t need any restrictions and even if an outbreak occurs it will die out by itself. Think of measles or polio. We don’t do anything to control their spread. Our vaccination rates are high enough to ensure any outbreak quickly dies.” added Dr. Rannan-Eliya.
“The level of vaccine protection needed to achieve herd immunity depends on two things: 1) Efficacy of vaccine preventing transmission, 2) Infectiousness of vaccine (R). Both matter.
“Higher #1 is, the lower the vaccine coverage needed. The higher the #2 is the higher the vaccine coverage needed. With the original virus, R was 2.5–3.5. We don’t have an exact value since it is quite hard to compute this once controls are put in place. But that’s the range of scientific estimates.
“AZ efficacy in preventing illness is 70%. We don’t have a good estimate of how effective it is in preventing transmission, but it won’t be higher than 70%. Assuming it is an optimistic 70%, and assuming that R is 2.5–3.5, AZ could achieve herd immunity with 86–102% coverage. The 102% number is if R is 3.5, which is not so likely. This conclusion is basic epidemiology. It’s not an opinion of mine. All the UK epidemiologists get the same number,” he explained.
"We still do not have data to show that there’s community transmission, but random testing should begin. Testing should at least be increased to 25,000 per day to detect more cases. People experiencing respiratory complications should definitely be tested. We estimate that around 50,000 patients visit orthopedic care services and testing should also be done in that capacity - Association of Laboratory Technologists President Ravi Kumudesh "
Dr. Rannan-Eliya further said that if B.1.1.7 is 43% more transmissible than the original virus (this is the bottom end of the range cited above), then the vaccine coverage level needed is 103-114%. “That is you have to vaccinate more than your whole population. Herd immunity is impossible. Obviously B.1.1.7 is probably more infectious than that, so I am being very conservative. Further even 90% coverage is very hard to achieve, since children are not approved for vaccination yet, and they amount to more than 10% of the population. What does this mean? It means that with AZ, the virus would continue to spread and kill people unless we have controls in place. That is we cannot have normality.
“I stress this is not an opinion. This is simply what the data mean. All the leading UK epidemiology groups plus the UK Government came to the same conclusion early this year. So the bottom line is that we cannot achieve herd immunity any longer with AZ. By letting in B.1.1.7 and not eliminating we have no choice, but to buy more expensive, better vaccines. The UK incidentally knows this which is why it announced this week it is buying an additional 50 million doses of Pfizer to give everyone in UK a third shot,” he added.
Asked about medical experts’ claims on informing authorities about the variant before New Year Dr. Rannan-Eliya said that SJU reported in February that it detected B.1.1.7 in four community samples collected in January- Colombo, Vavuniya and somewhere else. “So the April 8 detections are not the first ones. I think I can call myself a medical expert and also a public health expert, and I warned the authorities including the Secretary of Health, the Chief Epidemiologist and a minister that my analysis indicated that B.1.1.7 would become dominant by April, and that the outbreak would accelerate beyond control unless stringent actions were taken to stop the outbreak. Those warnings were given on 16 February 2021.
“This argument that medical experts informed on April 8 is irrelevant. By April 8, it was far too late. It takes 2-3 months for a few cases of B.1.1.7 to become dominant. It started in January. By the time the variant becomes most of your cases it is too late,” he said.“The medical community had enough information to predict all of this two months ago. So did MOH and the Government. In my view this is a scandal as bad as ignoring the intelligence on the Easter Bombings. The only difference is that B.1.1.7 may end up killing more Sri Lankans than the terrorists did,” he said.
He further said that with B.1.1.7 it is now much harder to control the virus. “All the control methods will work, but less effectively. Most methods cannot be increased. Eg: we can’t increase mask wearing beyond 100%. The only intervention that can bring transmission down and allow us to beat this is testing/contact tracing/isolation. We need to ramp up testing massively. We also need to stop all gatherings and stop all unnecessary indoor activities. A short lockdown to get these measures into place could help, but a lockdown by itself is not enough. We need first of all the testing,” he added.
Mixing vaccines
The Government announced that research has commenced on the possibility of mixing one COVID vaccine brand with another due to the existing shortage of vaccine supplies. In response Dr. Rannan-Eliya said that mixing vaccines may have two benefits. “It might improve the effectiveness of the individual vaccines which might not be so effective by themselves. Although the Chinese recently raised this idea, the original push to do this came from the UK, where AstraZeneca realised that the Russian Sputnik vaccine worked better than their Oxford one. AstraZeneca has said it wanted to see if mixing a single dose of AZ with a single dose of Sputnik would work better. I believe that clinical trials of doing this have started, with AZ working with the Russians. So it is a legitimate scientific idea, but as far as I know we do not have any clinical trial data yet to know how well it works with any combination of vaccines. So yes a legitimate idea, but one for which we currently have no scientific data on risks and benefits,” he said.
He further said that it may be an unavoidable workaround to interruption in supplies. “The benefit is that you can improve the impact of your first dose when the second dose of the first vaccine is not available, which must be balanced against the current scientific uncertainty on how effective this will be. The dictum that beggars can’t be choosers is quite apt,” he added.
PCR kits running out of stock?
With a higher number of cases being detected daily health officials observe a reduction in PCR testing kits. Association of Laboratory Technologists President Ravi Kumudesh said that during the next 10-15 days PCR testing should increase. “We still do not have data to show that there’s community transmission, but random testing should begin. Testing should at least be increased to 25,000 per day to detect more cases. People experiencing respiratory complications should definitely be tested. We estimate that around 50,000 patients visit orthopedic care services and testing should also be done in that capacity. But right now only 15,000 PCR tests are being done per day and that is also being done according to a slot system.” said Kumudesh.
“Another issue is the sensitivity of these testing kits. Our testing kits have less sensitivity. Therefore certain results might be negative. But if the same sample is tested from a kit with high sensitive, chances are that results may be positive. Therefore repeatability will increase,” he said.
He further said that there’s only one laboratory to do genetic sequencing. “The PCR kits we have cannot detect the different variants. The only kit that can detect variants is at the Sri Jayawardenapura University. On the other hand when doing a PCR test an extraction should be done. If this is done manually it takes around six hours. But the problem right now is that there are no reagents to do extractions,” he added.
When asked about the quantities that are remaining and the quantity that is required he claimed that there’s no sufficient data to give a direct answer. “This is why we have suggested that a technical committee be appointed to look into the technicalities at this critical hour.” he concluded. However, Health Minister Pavithra Wanniarachchi yesterday said in Parliament that PCR testing has been increased to 25,000 per day.
Several attempts to contact Director General of Health Services Dr. Asela Gunawardena to inquire on the quantities of PCR testing kits proved futile.
25 Dec 2024 7 minute ago
24 Dec 2024 9 hours ago
24 Dec 2024 24 Dec 2024
24 Dec 2024 24 Dec 2024
24 Dec 2024 24 Dec 2024