07 Oct 2024 - {{hitsCtrl.values.hits}}
| Mucormycosis is a life-threatening infection with a high mortality rate if not treated promptly |
| The infection primarily affects people with weakened immune systems or certain predisposing health conditions |

Mucormycosis is a severe, fungal infection caused by a group of moulds belonging to the order Mucorales. These fungi are commonly found in the environment, especially in soil, decaying organic matter, indoor or outdoor air, on food items and in dust. The infection primarily affects people with weakened immune systems or certain predisposing health conditions.
Risk factors
 Uncontrolled diabetes: Particularly with diabetic ketoacidosis is a major risk factor in the Asiatic region and globally. This poses a significant threat to the Sri Lankan population as well because according to a survey almost one in four Sri Lankan adults are diabetic.
Uncontrolled diabetes: Particularly with diabetic ketoacidosis is a major risk factor in the Asiatic region and globally. This poses a significant threat to the Sri Lankan population as well because according to a survey almost one in four Sri Lankan adults are diabetic.
Immunocompromised individuals: Those with weakened immune systems, such as people undergoing cancer treatment, organ transplant recipients, patients with haematological malignancies or those on high-dose steroids.
Patients with burn injuries, injection drug users and the extensive use of voriconazole are also considered risk factors.
COVID-19 patients: A surge in mucormycosis cases has been seen in some COVID-19 patients, especially those who were treated with steroids and had other risk factors like diabetes. This was evident in India.
Modes of transmission
Mucormycosis occurs when a person inhales the fungal spores – which can enter the sinuses or lungs – and when the fungus enters the body through broken skin, open wounds or by ingestion.
Causative agents
The fungi that cause mucormycosis include species like Rhizopus, Mucor, and Rhizomucor among many other species.
Clinical types of mucormycosis
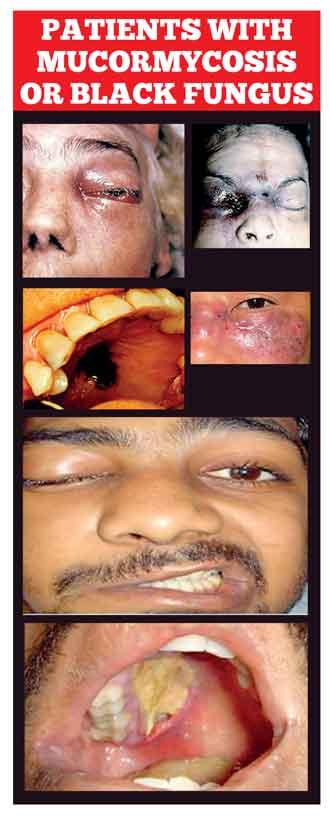
Rhino cerebral (sinus and brain): It is the commonest clinical form of mucormycosis. It initially affects the sinuses and can spread to the face, eye and brain.
Pulmonary (lung): This form primarily affects people with weakened immune systems, such as those with cancer or organ transplants. In Sri Lanka, most patients with pulmonary mucormycosis have uncontrolled diabetes mellitus.
Cutaneous (skin): Occurs when the fungus enters through a break in the skin, often after surgery, burns or trauma.
Gastrointestinal: This type is more common in premature infants or individuals with malnutrition.
Disseminated: When the infection spreads through the bloodstream to other organs like the brain, heart or spleen.
Symptoms
Symptoms depend on the type and area of infection:
Rhino cerebral: Facial swelling, black lesions on the nasal bridge or upper mouth, fever and headache.
Pulmonary: Fever, cough, chest pain and shortness of breath.
Cutaneous: Pain, swelling, skin redness and blackened or necrotic (dead) tissue at the site of the infection.
Gastrointestinal: Abdominal pain, nausea, vomiting and gastrointestinal bleeding.
Disseminated: Can cause a variety of symptoms depending on the organs affected, but generally results in mental confusion, coma and even death if untreated.
Diagnosis
Diagnosis typically involves a combination of clinical examination, biopsy of infected tissue and laboratory investigations including direct microscopy and culture, also imaging tests like CT or MRI scans to assess the extent of the infection.
Treatment
Antifungal medications: The mainstay of treatment is intravenous antifungal therapy.
Surgical intervention: Infected tissues need to be surgically removed, especially in cases involving the sinuses, brain or lungs.
Control of underlying conditions: Managing diabetes or reducing the use of immunosuppressive drugs is also critical in managing the infection.
Epidemiology
There is no decisive data pertaining to the incidence or prevalence of mucormycosis in Sri Lanka, and although a limited handful of research has been carried out more data and statistics are undeniably needed. The Medical Research Institute being the Reference Laboratory for Medical Mycology in Sri Lanka receives patient samples from hospitals in every Province in the country, and from first-hand experience we can perceive that there is a substantial amount of mucormycosis identified from these samples over the past few years.
Mucormycosis is a life-threatening infection with a high mortality rate if not treated promptly. Early diagnosis and treatment, including aggressive antifungal therapy and surgery, are crucial for improving outcomes.
(Dr. Sarah Makeen is a Senior Registrar in Medical Mycology at the Medical Research Institute in Colombo 8)
25 Dec 2024 9 hours ago
25 Dec 2024 9 hours ago
25 Dec 2024 25 Dec 2024