
World Kidney Day (WKD), observed annually on the 2nd Thursday in March, is a global health awareness campaign that emphasizes the importance of kidneys and aims to reduce the frequency and impact of kidney disease worldwide. Let’s delve into the history and significance of this crucial day:
and aims to reduce the frequency and impact of kidney disease worldwide. Let’s delve into the history and significance of this crucial day:
History of World Kidney Day:
The inaugural celebration of World Kidney Day took place in 2006.
The initiative was a collaborative effort between the International Society of Nephrology (ISN) and the International Federation of Kidney Foundations (IFKF).
The primary objective was to raise awareness about kidney-related conditions and their impact on
overall health.
During this month we as the health professionals at the National Institute for Nephrology, Dialysis and Transplantation hope to educate the public about kidney diseases.
At least 1 in 10 people worldwide suffer from kidney disease. Only 40% and 60% of those with hypertension and diabetes are aware of their diagnosis, and far smaller proportions are receiving treatment and at target goals. Moreover, at least 1 in 5 people with hypertension and 1 in 3 with diabetes suffer Chronic Kidney Disease (CKD).
Here is Dr. Rajeev Menon – Medical Officer from the National Institute for Nephrology, Dialysis and Transplantation, Colombo in discussion with Senior Consultant Nephrologist from the same Institute Dr. Anura Priyantha Hewageegana.
Q How do you define a kidney disease?
A kidney disease is said to exist when the functions of the kidneys are impaired (mainly excretory). The impairment of function may be short lived, reversible or permanent. When it is reversible we call it an ‘Acute Kidney Injury’ while a permanent impairment is termed ‘Chronic Kidney Disease’ (CKD). CKD is responsible for the highest morbidity and mortality from any given renal illness.
Q What is Chronic Kidney Disease (CKD)?
It is a progressive and permanent decline in renal functions over a period of time exceeding three months. As it is a permanent loss of function it is not possible to regain the lost functional capacity. Further, the disease is progressive (You cannot halt the functional decline over time). The only achievement with treatment is to retard the functional decline, by controlling the risk factors governing the disease progression. It progresses gradually from its early stages (stage1 & 2) to more serious stages ( stage 5) requiring replacement treatment like dialysis and transplantation.
Q How is it diagnosed?
As in any other disease, CKD is diagnosed taking a clinical history, arranging a physical examination of the patient and proceeding to lab investigations. It is noteworthy that the disease is symptom free until it progresses to advanced stages, and therefore the early stages are missed in most cases complicating its management.
Some patients are unaware of any kidney impairment until they reach End Stage Chronic Kidney Disease (ESKD).
Therefore high risk individuals should be screened without waiting until symptoms of CKD develop. This applies to patients with a non communicable disease like diabetes and or hypertension, chronic kidney infections, stones and patients with urinary abnormalities.
After a clinical conclusion (history, physical examination) it is advised to arrange lab investigations systematically starting from urinalysis, blood biochemistry (blood urea, serum creatinine, estimated glomerular filtration rate) and imaging. (ultrasound evaluation of the kidneys).
Patients are usually found to have proteinuria, high blood urea, serum creatinine and chronic structural changes of kidneys signifying CKD.
CKD has a wide spectrum from CKD stage 1 to stage 5 based on the filtration capacity called glomerular filtration rate (GFR).
Patient’s filtration capacity is grossly impaired (and therefore require external support either in the form of dialysis or transplantation) during the terminal stages of CKD.
Q What causes CKD?
The major cause of CKD in any country (high income/ low income) is the growing epidemic of non communicable diseases (NCDs) such as diabetes (both type 1 & 2) and hypertension. Chronic kidney infections (chronic pyelonephritis), chronic urinary tract obstructions (due to kidney stones or prostate enlargement), congenital conditions like cystic diseases (polycystic kidneys), chronic glomerular nephritis/vasculitis (inflammation in kidney substance and blood vessels), toxins (environmental, animal and plant toxins) are other major causes.
Sometimes the cause of CKD is not evident.
The Chronic interstitial nephritis in agricultural communities (CINAC) prevailing in the North Central region of Sri Lanka is thought to be multi-factorial.
Q Who are at risk of CKD?
- Diabetes (both type 1&2) and hypertension are the more common causes of CKD in most adults. Other risk factors include,
- Family history of CKD
- Obesity
- Smoking
- Heart Disease
- Inherent Kidney Diseases
- Past history of damage to the kidneys
- Advancing age.
Q How to prevent CKD
- A diabetic or hypertensive patient should get appropriate treatment to targets.
- Quit smoking
- Restrict salt/sugar/ starch
- Moderate alcohol
- Refrain from using over the counter pain medications and antibiotics
- Regular exercise
- Good volumes of liquids a day
- Wholesome meal
- High risk category persons should get an early screening.
- Regular recreational activity
Q How is CKD treated?
Chronic Kidney Disease (CKD) has a wider spectrum from grade 1 to grade 5, based on the glomerular filtration capacity (GFR).
Early stages of CKD are treated with medications along with health lifestyle modifications. Drug treatment of diabetes, high blood pressure and proteinuria is pivotal. As the disease progresses, complications like bone illness and anemia emerge, requiring treatment. During the later stages of CKD treatment involves medications to control symptom burden of CKD (eg: swelling of legs). When the functioning of the kidney is negligible a replacement is required. Kidney replacement is two-fold (a) Dialysis (b) Transplantation.
Q What is the role of dialysis and transplantation in CKD?
Dialysis involves blood purification (removal of nitrogenous waste substances) using a machine, when the native kidneys are unable to provide excretory functions adequately. Excess water and nitrogenous waste products like urea and creatinine are filtered and acid – base status in the body is restored following dialysis. On average a patient requires 2-3 dialysis sessions per week until a successful kidney transplantation or lifelong if kidney transplantation is not considered. Dialysis improves survival and controls symptoms of CKD.
There are 2 broad forms of dialysis.
1. Hemodialysis - Blood purification using a machine and an extra corporeal blood circuit.
2. Peritoneal dialysis – Blood purification involving a solute exchange between an instilled chemical solution and abdominal blood vessels within the abdominal cavity.
There is no inferiority of any form of dialysis over the other if chosen for the correct clinical setting. The form of dialysis chosen for any given patient is through a shared decision making involving the kidney specialist, patient and family. Both the medical factors and patient preferences are considered in decision making.
Kidney transplantation is considered as the last viable option for end stage Chronic Kidney Disease.( for eligible patients)
Some patients are unsuitable for this option on medical grounds. The medical team will enlighten the patients and families regarding their candidacy for kidney transplantation or dialysis during the family counselling sessions.
If a patient is suitable for kidney transplantation, he/she should choose it as the best option for kidney replacement therapy. Some patients though unsuitable for kidney transplantation are suitable for dialysis. They should opt for this option as their best modality of kidney replacement treatment. Patients who are unsuitable for any of the above modalities invariably have to be on drug treatment (as conservative therapy) as this is the only option left for them.
Q How do you select patients for dialysis or kidney transplantation?
The decision regarding the modality of therapy is dependent on patient’s medical suitability and his/her wishes. The medical suitability is decided by the treating medical team. The medical suitability is dependent on age and the presence of concomitant other major organ illness.
A medically suitable person can refuse any modality of kidney replacement provided that it is a well informed decision.
Q Can drugs cure CKD?
CKD has no definite cure with drugs, though CKD can be controlled with drugs.
The progression of CKD can be retarded with medications. The complications and symptoms of CKD can be managed with drugs. Still, restoration of already lost functions is not possible. Halting of disease progression also is impossible with drugs.
Q What are the options available for patients not qualifying for dialysis and kidney transplantation?
They should invariably be on medical management with drugs for their symptoms control, management of complications and preservation of residual kidney function. This is called comprehensive conservative management. It is extremely important to control the symptom burden of CKD and focus on their end-of-life care. This branch of medicine is called Palliative care.
Q Can anti diabetic drugs cause kidney diseases?
Definitely not. Judicious use of anti diabetics prevent kidney diseases/ help preserve kidney function.
Q Should all patients undergo a period of dialysis before a kidney transplantation?
Not a requirement.
Q Should you remove the native kidneys before a transplant?
No we leave them intact.
Q How should a post kidney transplant patient protect his/ her grafted kidney?
- They should take their prescribed medications (specially immunosuppressive drugs) regularly according to medical advice.
- They should control their diabetes/hypertension well
- They need periodic lab testing
- They should adopt a healthy lifestyle
- They should protect themselves from infections ( take precautions to avoid associating with infectious patients and their contacts)
- They should get vaccinations according to medical advice.
Q As a senior Consultant in Nephrology seeing so many CKD patients in your life what is your advice to Sri Lankans?
- If you are a patient with non communicable diseases (NCD) check your kidneys regularly.
- Control your diabetes and hypertension to targets.
- If you are in a high risk category check your kidneys regularly.
- Adopt a healthy lifestyle to prevent NCDs.
- Do not disregard abnormalities in urinalysis ( eg: slight proteinuria/ trace of blood in urine).
- Healthy dietary modifications like salt/sugar restrictions.
- Healthy lifestyle measures like;
Quitting smoking
Moderate intake of alcohol
Regular exercise and recreational activities should be encouraged.
Dr. Anura Priyantha Hewageegana
MBBS, MD, FCCP
Senior Consultant Nephrologist
National Institute for Nephrology, Dialysis and Transplantation.
Colombo.
Living well with kidney disease: Navigating challenges and empowering lives
- Encourage open conversations within the family. Share feelings, fears, and hopes
- Create a budget that accounts for medical expenses. Explore financial assistance programmes if needed
- Arrange for breaks to prevent caregiver burnout
- Consider counseling or therapy to manage stress and emotions
Chronic Kidney Disease (CKD) is a condition that affects millions of people worldwide. It not only impacts the individual’s health but also places a significant burden on their family members. In this article, I will explore how CKD affects well-being, discuss the challenges faced by patients and their families, and provide practical tips for overcoming these difficulties.
members. In this article, I will explore how CKD affects well-being, discuss the challenges faced by patients and their families, and provide practical tips for overcoming these difficulties.
Knowledge is power when it comes to managing CKD. Understanding your condition, treatment options, and how to prevent complications can give you a sense of control. Work closely with your healthcare team to learn as much as you can about CKD and its management.
The impact on well-being
CKD often leads to symptoms such as fatigue, weakness, and fluid retention. These physical discomforts can affect an individual’s overall quality of life.
Physical Discomfort:
: Coping with a chronic illness can be emotionally draining. Anxiety, depression, and feelings of helplessness are common among CKD patients and their families.
Financial Strain:
The cost of medications, dialysis, and other treatments can strain family finances. Balancing medical expenses with daily living costs becomes a challenge.
CKD necessitates lifestyle modifications. Patients may need to alter their diet, restrict certain activities, and adhere to medication schedules. These adjustments impact both the patient and their family members.
Lifestyle Changes
The burden on families
Caregiver Stress: Family members often take on the role of caregivers. The demands of care-giving can lead to stress, exhaustion, and feelings of isolation.
Emotional Impact: Witnessing a loved one struggle with CKD can evoke feelings of helplessness, guilt, and sadness. Family members may worry about the patient’s well-being constantly.
Social Isolation: Patients may withdraw from social activities due to their health condition. This isolation affects not only the patient but also their family’s
social life.
Work and Productivity: Family members may need to take time off work to care for the patient. This can impact their own career and financial stability.
Strategies for overcoming challenges
Education and Empowerment:
Patient Education: Understanding CKD, its progression, and treatment options empowers patients to actively participate in their care.
Family Involvement: Educate family members about CKD, its impact, and ways they can support the patient.
Emotional Support:
Open Communication: Encourage open conversations within the family. Share feelings, fears, and hopes.
Support Groups: Joining support groups provides emotional support and helps family members connect with others facing similar challenges.
Financial Planning:
Budgeting: Create a budget that accounts for medical expenses. Explore financial assistance programmes if needed.
Insurance Coverage: Understand insurance policies and coverage related to CKD treatments.
Self-care for caregivers:
Respite Care: Arrange for breaks to prevent caregiver burnout.
Seek Professional Help: Consider counseling or therapy to manage
stress and emotions.
Promoting Wellness:
Healthy Lifestyle: Encourage the patient to follow a kidney-friendly diet, stay hydrated, and engage in regular physical activity.
Early Detection: Regular check-ups help detect CKD early, allowing for timely interventions.
Conclusion
Living well with kidney disease requires a holistic approach. By empowering patients and their families, promoting education, and addressing emotional and financial challenges, we can improve the well-being of those affected by CKD. Let us strive for a world where kidney health is a priority for everyone, everywhere.
Navigating life with chronic kidney disease is a journey of adaptation and resilience. With the right knowledge, support, and mindset, you can manage your condition effectively and lead a fulfilling life.
Remember, you are not alone in this journey. Reach out to your healthcare team, support networks, and loved ones. Together, we can overcome the challenges posed by kidney disease and lead
fulfilling lives.
Dr. Rajeev Menon, a Medical Officer in Anesthesia and Intensive Care at the National Institute for Nephrology, Dialysis and Transplantation has an insatiable thirst for knowledge and a passion for sharing it.
Every day presents a new opportunity to learn something that can enhance my practice and benefit my patients. With the ever-evolving landscape of medicine, I believe that staying updated with the latest research and advancements is not just a professional responsibility but also a personal joy. Through my social media channels, I aim to demystify complex medical topics, provide valuable health tips, and foster an informed community. He is also the incumbent Secretary of the Clinical Travel Medicine Association
of Sri Lanka.
Nutrition considerations in chronic kidney disease
kidneys play a crucial role in filtering waste and excess fluids from the blood, as well as regulating levels of electrolytes like sodium, potassium, and phosphorus. When the kidneys are damaged, they may not be able to perform these functions effectively, leading to a build-up of waste products and imbalances in nutrient levels.
phosphorus. When the kidneys are damaged, they may not be able to perform these functions effectively, leading to a build-up of waste products and imbalances in nutrient levels.
This can impact a patient’s nutritional status and overall health, making it important to follow a specialized diet to help manage these imbalances and support kidney function.
However, exact nutritional application should be tailor made to each patient, as each patient’s condition (Co-existence of Diabetes, High blood pressure) is highly individual. Restrictions of diet also depend on the stage of the disease or how bad is the disease. In early stages of the disease the patient can be on a more flexible diet and undue restrictions may even hamper the patient’s well-being. Therefore, it is essential to discuss these restrictions with a nutrition specialist and a nephrologist before making changes in the diet.
This article aims to discuss general nutritional considerations of moderate to severe kidney disease in adults.
The diet in a patient with kidney disease should be able to prevent under nutrition while helping to reduce the workload on their kidneys and maintain overall health. This typically involves limiting certain nutrients such as sodium, phosphorus, and potassium, while also ensuring they get adequate protein and calories.
Some general principles for dietary intake in advanced kidney disease are as below.
Limiting sodium intake to help control blood pressure and reduce fluid retention.
Monitoring phosphorus intake, as high levels can lead to bone and heart problems.
Managing potassium levels, as too much potassium can be harmful for the heart.
Ensuring adequate protein intake, but not excessive amounts.
Let’s see how we could address each of them Limiting salt intake in diet:
Always read food labels: choose low-sodium or sodium-free options whenever possible.
Cook at home: Prepare meals at home using fresh ingredients, and spices instead of relying on pre-packaged or processed foods, which tend to be high in sodium.
Limit processed foods: Avoid or reduce consumption of processed foods like canned soups, deli meats, and fast food, as they are often high in sodium.
Use condiments and spices to flavour the food instead of salt
Be mindful when dining out: ask for dishes to be prepared without added salt, sauces on the side, and opt for steamed or grilled options instead of fried foods.
Be cautious with condiments like soy sauce, ketchup, and salad dressings, as they can be high in sodium.
Be mindful about phosphate levels
- Limit high-phosphorus foods: Avoid or limit foods that are high in phosphorus, such as dairy products, nuts, seeds, whole grains, and processed foods. You will have to get advice on restricting meat and fish which are high in phosphate but, at the same time are important sources of good quality proteins. Unnecessary restrictions in animal sources of protein can worsen the overall health of the person.
- Choose low-phosphorus alternatives: like white bread, rice, pasta, and fruits and vegetables with lower
- phosphorus content.
- Soak or leach high-phosphorus foods: high-phosphorus foods like beans, lentils, or certain vegetables, soaking or leaching them before cooking can help reduce their phosphorus content.
- Avoid phosphorus additives: Be cautious of phosphorus additives in processed foods, such as phosphoric acid in sodas and certain food preservatives.
- Take phosphate binders: phosphate binders can help control phosphorus levels by binding to phosphorus in the gut and preventing its absorption.
- Managing potassium intake from food
- Monitor potassium intake: Keep track of your potassium intake by reading food labels and being aware of high-potassium foods such as bananas, oranges, potatoes, tomatoes, and dairy products.
- Choose low-potassium foods: like green apples, berries, cabbage, green beans, and rice. You need to be aware of the safe quantities of these food to avoid high potassium intake. A nutrition specialist can guide you with this.
- Cook fruits and vegetables: can help reduce their potassium content. Use large amount of water in the pot when cooking or boiling to enhance potassium loss. Soaking or leaching high-potassium foods like potatoes or certain vegetables before cooking can help lower their potassium
- levels further.
- Limit potassium additives: Be cautious of potassium additives in processed foods, such as potassium chloride in salt substitutes and certain packaged foods.
- Avoid high-potassium salt substitutes: Some salt substitutes contain high levels of potassium, so it’s important to choose low-potassium alternatives if needed.
- Take medications as prescribed: If your healthcare provider prescribes medications to help manage potassium levels, be sure to take them as directed.
Ensure adequate protein intake in kidney disease
- Choose high-quality protein sources: Opt for high-quality protein sources such as lean meats, poultry, fish, eggs, and dairy products. These sources provide essential amino acids without adding excessive strain on the kidneys.
- Monitor portion sizes: Be mindful of portion sizes when consuming protein-rich foods to avoid consuming more protein than your body needs. Your nutrition specialist can guide you on this.
- Spread protein intake throughout the day: Instead of consuming a large amount of protein in one meal, try to spread your protein intake evenly throughout the day
- Consider plant-based protein sources: Incorporate plant-based protein sources like beans, lentils, tofu, and quinoa into your diet to vary your protein intake. Again, the quantities have to be guided.
- Limit phosphorus-rich protein sources: Some protein sources, such as dairy products and nuts, are high in phosphorus, which can be problematic for individuals with kidney disease. Be mindful of your phosphorus intake while choosing protein sources.
As an adult, controlling your weight in a healthy range avoiding unhealthy fat (eg: saturated oil) and carbohydrates (eg: simple sugars, refined flour) and being active as much as possible, will lay a foundation to a healthy life, preventing chronic kidney disease and all other none communicable diseases such as diabetes, hypertension and cancers.
Dr Manoji Gamage
MBBS,MSc,MD (Clinical Nutrition)
Consultant Nutrition Physician
National Institute of Nephrology Dialysis and transplant

 and aims to reduce the frequency and impact of kidney disease worldwide. Let’s delve into the history and significance of this crucial day:
and aims to reduce the frequency and impact of kidney disease worldwide. Let’s delve into the history and significance of this crucial day: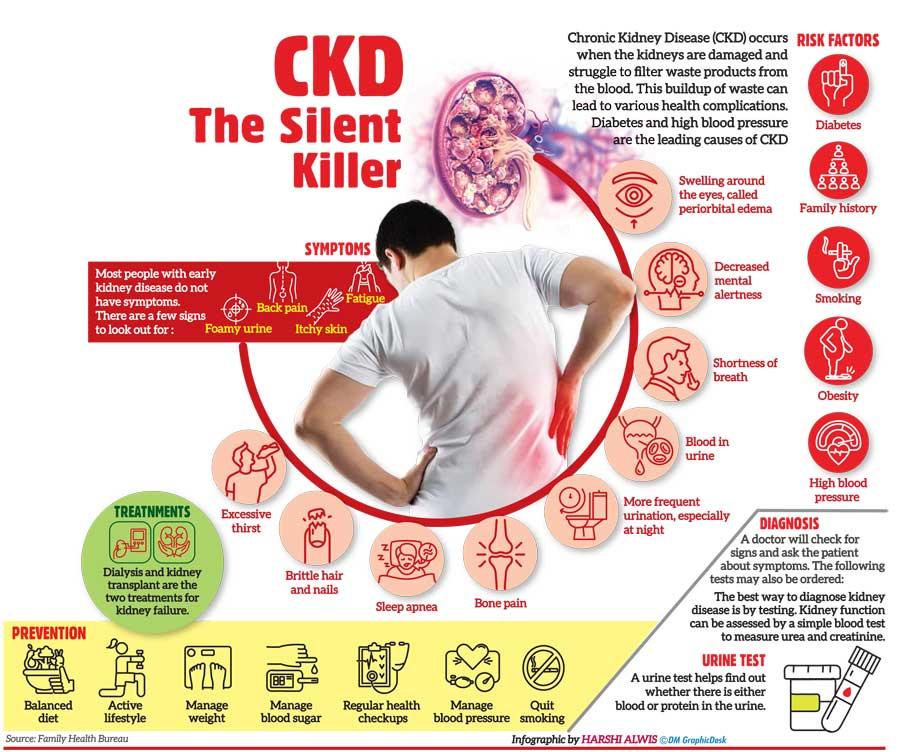
 members. In this article, I will explore how CKD affects well-being, discuss the challenges faced by patients and their families, and provide practical tips for overcoming these difficulties.
members. In this article, I will explore how CKD affects well-being, discuss the challenges faced by patients and their families, and provide practical tips for overcoming these difficulties. phosphorus. When the kidneys are damaged, they may not be able to perform these functions effectively, leading to a build-up of waste products and imbalances in nutrient levels.
phosphorus. When the kidneys are damaged, they may not be able to perform these functions effectively, leading to a build-up of waste products and imbalances in nutrient levels.