26 Mar 2021 - {{hitsCtrl.values.hits}}
 Ever thought that a simple pain in the scrotum with or without trauma, not addressed on time can result in permanent sub-fertility? Sounds scary, but that is the bitter truth behind testicular torsion-which is a serious surgical emergency, accounting for at least 0.5% of all the cases and one quarter of the scrotal complaints, presenting to the emergency department.
Ever thought that a simple pain in the scrotum with or without trauma, not addressed on time can result in permanent sub-fertility? Sounds scary, but that is the bitter truth behind testicular torsion-which is a serious surgical emergency, accounting for at least 0.5% of all the cases and one quarter of the scrotal complaints, presenting to the emergency department.
“Testicular torsion is mostly seen perinatally and in adolescence age. Although the exact causative factor is quite unclear, an abnormality in processus vaginalis, a blind‐ended evagination of the abdominal wall that develops during fetal life and typically undergoes obliteration during early life, is observed in most cases” says Dr Malaka Ranaweera (MBBS,MD,MRCS), Senior Registrar in General Surgery, Teaching Hospital Kurunegala.
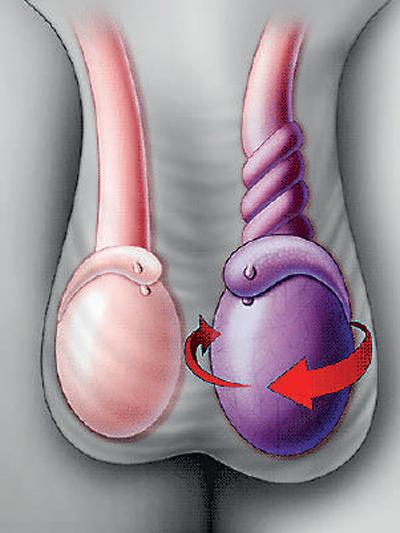 Testicular torsion occurs as the ultimate result of twisting of blood vessels together with the spermatic cord, which is the structure hangs the testes inside the scrotum. Other causes include trauma and exposure to cold temperature.
Testicular torsion occurs as the ultimate result of twisting of blood vessels together with the spermatic cord, which is the structure hangs the testes inside the scrotum. Other causes include trauma and exposure to cold temperature.
“When the testicle twists around the spermatic cord, the venous blood flow to it, gets obstructed giving rise to venous congestion eventually causing arterial flow to get obstructed and testicular ischemia. In simpler terms, this will result in both functional and structural deformity of the testicle, after which the entire structure becomes tender and swollen resulting in further twisting, like a vicious cycle with ultimate necrosis or permanent death of the organ” says Dr Ranaweera.
Testicular torsion often presents as an acute onset unilateral pain in the scrotum, lower abdomen or inguinal region associated with nausea and vomiting.
Usually, when a patient with a similar complaint presents, the first thing doctors do after taking a thorough history about the incident is carrying out an examination to see if the position of the testicle has changed with or without swelling and redness of the area.
Absence of Cremasteric reflex-contraction of the cremasteric muscle, pulling the scrotum and testis superiorly on the side upon, stroking the medial part of the thigh in a downward direction and the Prehn sign-relief of pain on elevating the testicle, were used to diagnose Testicular torsion decades back, but barely used now due to low sensitivity.
 TWIST to assess the twist
TWIST to assess the twistThe scoring system TWIST is used by certain clinicians in some centers to evaluate the presence of testicular torsion.
Hard testis - 2
Swelling - 2
Nausea/vomiting - 1
Absent cremasteric reflex - 1
High riding testis - 1
“When TWIST score is high, (5 or 6) the diagnosis of torsion is considered to be quite likely and surgery can be carried out even without an ultrasound scan-scrotum to avoid unnecessary delay in mandatory surgical exploration” explains Dr Ranaweera.
“As health care professionals, our main motive on patients presenting to us is to minimize serious complications of any pathology by carrying out the most important steps in a minimal amount of time. In that case, we focus on the other possibilities, which can present in a similar manner-which we call differential diagnosis. Torsion of the testicular appendages, epididymytis, orchitis, inguinal hernia, symptomatic hydrocele, testicular necrosis due to other causes and scrotal hematoma can give rise to symptoms which mimic Testicular torsion, so apart from the history and clinical examination, blood and imaging investigations would be of extreme to rule them out especially in an atypical presentation” he adds.
Ultra Sound scan-Scrotum which owns at least 93% sensitivity and 100% specificity used to play the hall mark in diagnosing Testicular torsion. However, according to latest research guidelines, this might not be very sensitive in neonates as 40% of neonatal testicles may have no apparent color flow doppler. Therefore, it is always better to look for expert advice immediately, in order to avoid serious complications.
Treatment of choice for Testicular torsion is a surgical exploration and untwisting the testes if it is viable. This is an emergency surgery done under general anesthesia or spinal anesthesia specially when it comes under the ceiling of “6” hours. Sometimes even before fasting is completed you are taken for the surgery after taking necessary precautions as viability of testes is time dependent.
Non-viable or necrosed testicles have to undergo Orchidectomy (20-40% of total cases) and contra-lateral orchiopexy is always done to prevent future torsion during the same operation or as an interval procedure.
“The typical window of opportunity for surgical intervention and testicular salvage is classically six hours from the onset of pain” says the doctor. Those who present within the first six hours of symptoms, own a salvage rate of nearly 100% but this number comes to less than 50%, if the delay is more than 12-24 hours.
The earlier you rush to the hospital and get yourself evaluated; the more chances you would own to get rid of unwanted complications.
“So, the take home message is to see immediate medical advice if you experience a similar presentation, especially if you are a young adult as what you go through might not be just a simple gastroenteritis or a urinary infection, but a debilitating condition which can completely take your potential in making babies away which of course is extremely serious as the statement itself sounds!” Dr Ranaweera underscores.
21 Dec 2024 27 minute ago
21 Dec 2024 2 hours ago
21 Dec 2024 5 hours ago
21 Dec 2024 5 hours ago
21 Dec 2024 6 hours ago